Mechanism of Breathing and Exchange of Gases | Biology Class 11 - NEET PDF Download
| Table of contents |

|
| Mechanism of Breathing |

|
| Inspiration |

|
| Expiration |

|
| Respiratory Volumes and Capacities |

|
| Exchange of Gases |

|
Mechanism of Breathing
Breathing has two stages: Inspiration (inhaling air) and Expiration (exhaling air). Movement of air is due to the pressure gradient between the lungs and the atmosphere.
Inspiration
Inspiration happens when the intra-pulmonary pressure is lower than atmospheric pressure, creating a negative pressure inside the lungs.
Steps involved:
- Diaphragm contracts: Increases the volume of the thoracic cavity along the antero-posterior axis.
- External intercostal muscles contract: Lifts the ribs and sternum, increasing thoracic volume along the dorso-ventral axis.
- Increased thoracic volume leads to increased pulmonary volume, lowering intra-pulmonary pressure.
- Air flows into the lungs due to this pressure difference.
 Inspiration
Inspiration
Expiration
Expiration occurs when intra-pulmonary pressure becomes higher than atmospheric pressure.
Steps involved:
- Diaphragm and intercostal muscles relax: The diaphragm and sternum return to their normal positions.
- Thoracic and pulmonary volumes decrease, causing intra-pulmonary pressure to increase.
- Air is expelled from the lungs as a result.
 Expiration
Expiration
Muscle Involvement: Diaphragm and intercostal muscles (external and internal) are key for generating pressure gradients. Additional abdominal muscles can be used to enhance both inspiration and expiration.
Breathing Rate and Measurement: A healthy human breathes 12-16 times per minute. The volume of air during breathing can be measured with a spirometer, which helps assess pulmonary function.
Respiratory Volumes and Capacities
- Tidal Volume (TV): The amount of air inhaled or exhaled during a normal breath, which is about 500 mL. A healthy person can breathe in or out approximately 6000 to 8000 mL of air per minute.
- Inspiratory Reserve Volume (IRV): The extra volume of air that can be inhaled with force after a normal inhalation, averaging between 2500 mL to 3000 mL.
- Expiratory Reserve Volume (ERV): The additional volume of air that can be exhaled with force after a normal exhalation, averaging between 1000 mL to 1100 mL.
- Residual Volume (RV): The volume of air remaining in the lungs after a forcible exhalation, averaging between 1100 mL to 1200 mL.
By combining various respiratory volumes, different pulmonary capacities can be derived, which are useful in clinical diagnosis.
- Inspiratory Capacity (IC): The total volume of air that can be inhaled after a normal exhalation, calculated as TV + IRV.
- Expiratory Capacity (EC): The total volume of air that can be exhaled after a normal inhalation, calculated as TV + ERV.
- Functional Residual Capacity (FRC): The volume of air remaining in the lungs after a normal exhalation, calculated as ERV + RV.
- Vital Capacity (VC): The maximum volume of air that can be inhaled after a forced exhalation, or the maximum volume of air that can be exhaled after a forced inhalation. This includes ERV, TV, and IRV.
- Total Lung Capacity (TLC): The total volume of air that can be accommodated in the lungs at the end of a forced inhalation, which includes RV, ERV, TV, and IRV, or VC + RV.
Exchange of Gases
Gas exchange primarily occurs in the alveoli, where O2(oxygen) and CO2(carbon dioxide) are exchanged between the blood and the tissues through a process called diffusion. This process relies on the difference in partial pressure or concentration gradient between the gases. Partial pressure is the pressure exerted by an individual gas in a mixture, indicated as pO2 for oxygen and pCO2 for carbon dioxide.
 Partial Pressures (in mm Hg) of Oxygen and Carbon dioxide at Different Parts Involved in Diffusion in Comparison to those in Atmosphere
Partial Pressures (in mm Hg) of Oxygen and Carbon dioxide at Different Parts Involved in Diffusion in Comparison to those in Atmosphere
- The rate of diffusion can be influenced by factors such as the solubility of the gases and the thickness of the membranes involved in the diffusion process.
- In the alveoli, there is a concentration gradient that facilitates the movement of oxygen from the alveoli into the blood and subsequently into the tissues. Conversely, carbon dioxide moves from the tissues into the blood and then into the alveoli.
- Although the concentration gradient for carbon dioxide is in the opposite direction, its higher solubility (20-25 times greater than that of oxygen) allows it to diffuse more readily through the membrane.
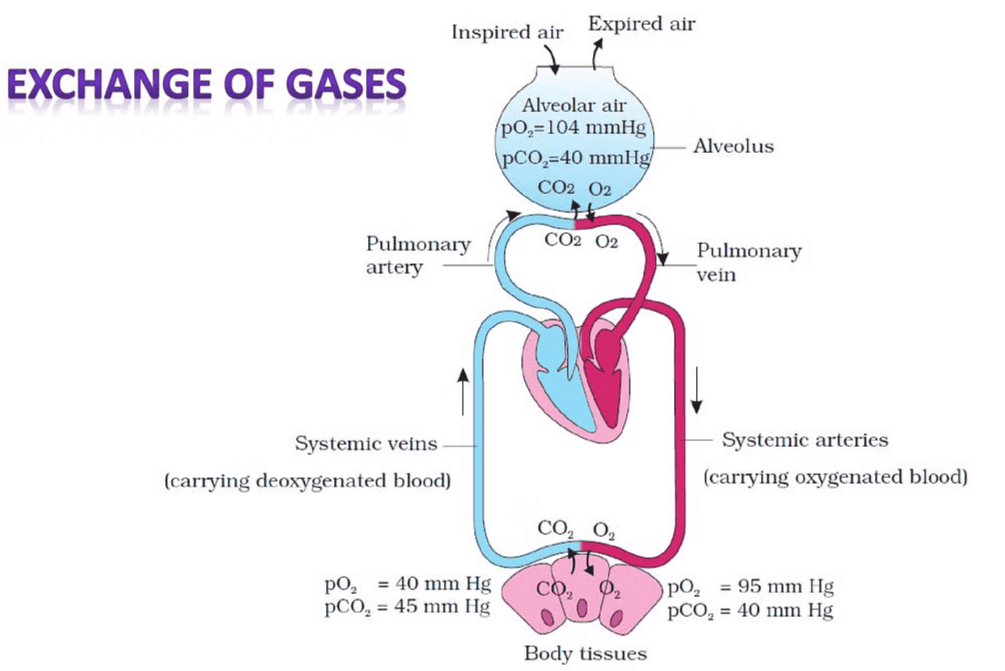 Diagrammatic representation of exchange of gases at the alveolus and the body tissues with blood and transport of oxygen and carbon dioxide
Diagrammatic representation of exchange of gases at the alveolus and the body tissues with blood and transport of oxygen and carbon dioxide
The diffusion membrane consists of three main layers:
- Thin squamous epithelium of the alveoli
- Endothelium of the alveolar capillaries
- Basement substance, which includes a thin basement membrane supporting the squamous epithelium and the basement membrane surrounding the endothelial cells of the capillaries
A Diagram of a section of an alveolus with a pulmonary capillary.The total thickness of this membrane is less than a millimeter, making it conducive for the diffusion of gases.
Overall, the conditions in the body are optimal for the diffusion of oxygen from the alveoli to the tissues and the diffusion of carbon dioxide from the tissues to the alveoli.
|
180 videos|362 docs|148 tests
|
FAQs on Mechanism of Breathing and Exchange of Gases - Biology Class 11 - NEET
| 1. What is the mechanism of inspiration in breathing? |  |
| 2. How does expiration occur in the breathing process? |  |
| 3. What are the different respiratory volumes and capacities? |  |
| 4. How is gas exchange facilitated in the lungs? |  |
| 5. What role do the respiratory muscles play in breathing? |  |




















