Mechanism of Urine Formation & Concentration of Filterate | Biology Class 11 - NEET PDF Download
Urine formation is a complex physiological process primarily carried out by the kidneys, vital organs responsible for filtering waste products from the blood and regulating the body's fluid balance. The process of urine formation involves several key steps:
Steps Involved in Urine Formation
Urine formation begins with glomerular filtration, where blood is filtered to create a fluid called filtrate. Reabsorption then occurs in various parts of the nephron to retrieve essential substances, while secretion removes additional waste products and helps maintain pH balance. These processes collectively lead to the formation of urine, which is ultimately excreted from the body.
The mechanism of urine formation involves three steps or processes :
(I) Glomerular filtration
(II) Selective tubular reabsorption
(III) Tubular secretion
1. Glomerular Filtration
- Initial Step: Blood filtration is the first step in urine formation, carried out by the glomerulus.
- Filtration Rate: On average, kidneys filter 1100-1200 ml of blood per minute, about 1/5th of the blood pumped by each heart ventricle.
- Filtration Process: Blood is filtered through three layers: the endothelium of glomerular blood vessels, the basement membrane, and the epithelium of Bowman’s capsule.
- Podocytes: The epithelial cells of Bowman’s capsule, called podocytes, have intricate arrangements with filtration slits, allowing only certain substances to pass.
- Ultra Filtration: This process is so fine that almost all plasma constituents except proteins pass into the Bowman’s capsule lumen.
- Glomerular Filtration Rate (GFR): GFR measures the amount of filtrate formed per minute, with a healthy GFR being approximately 125 ml/minute or 180 litres per day.
Regulation of GFR
- Juxta Glomerular Apparatus (JGA): JGA is a specialized region formed by modifications in the distal convoluted tubule and the afferent arteriole.
- Role of JGA: When GFR falls, JG cells release renin, stimulating glomerular blood flow and restoring GFR to normal.
2. Reabsorption
- Process Overview: Nearly 99% of the filtrate (180 litres per day) is reabsorbed by renal tubules, with only 1.5 litres released as urine.
- Mechanisms: Reabsorption occurs through active or passive mechanisms in different nephron segments.
- Active Reabsorption: Substances like glucose, amino acids, and Na+ are reabsorbed actively.
- Passive Reabsorption: Nitrogenous wastes are absorbed by passive transport, and water is reabsorbed passively in the initial nephron segments.
3. Tubular Secretion
- Role in Urine Formation: Tubular secretion involves the secretion of substances like H+, K+, and ammonia into the filtrate.
- Importance: This process helps maintain the ionic and acid-base balance of body fluids.
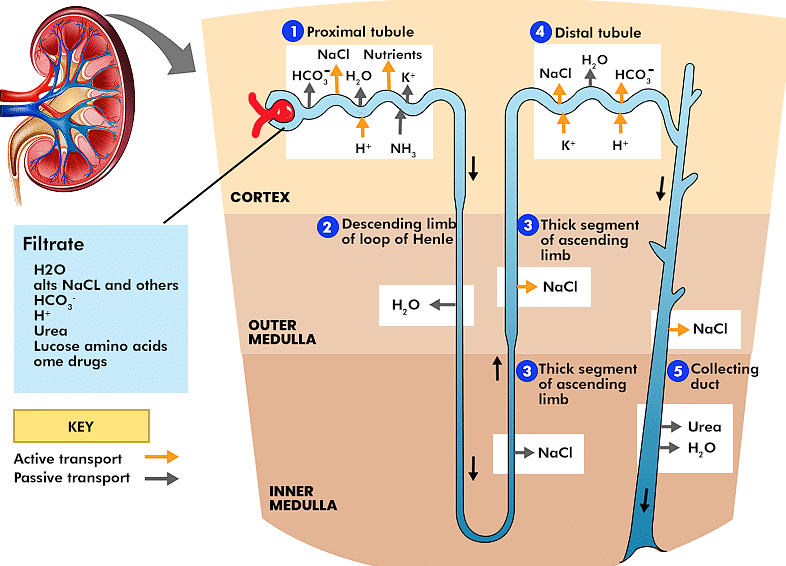
Function of the Tubules
(i) Proximal Convoluted Tubule (PCT): The PCT is lined with simple cuboidal brush border epithelium, which increases the surface area for reabsorption. This segment reabsorbs nearly all essential nutrients and 70-80% of electrolytes and water. The PCT also helps maintain the pH and ionic balance of body fluids by selectively secreting hydrogen ions and ammonia into the filtrate and absorbing HCO3 from it.
(ii) Henle's Loop:
- Descending Limb: This limb is permeable to water but nearly impermeable to electrolytes. As a result, water is reabsorbed, and the filtrate becomes more concentrated as it moves down.
- Ascending Limb: This limb is impermeable to water but allows the active or passive transport of electrolytes. As the concentrated filtrate moves upward, it gets diluted due to the passage of electrolytes into the medullary interstitial fluid. The ascending limb plays a crucial role in maintaining the high osmolarity of the medullary interstitial fluid.
(iii) Distal Convoluted Tubule (DCT): In the DCT, the reabsorption of Na+ and water is conditional. This segment is also capable of reabsorbing HCO3 and selectively secreting hydrogen and potassium ions and ammonia to maintain the pH and sodium-potassium balance in the blood.
(iv) Collecting Duct: The collecting duct extends from the cortex of the kidney into the inner parts of the medulla. It allows for the reabsorption of large amounts of water, producing concentrated urine. This segment also permits the passage of small amounts of urea into the medullary interstitium to help maintain osmolarity. Additionally, it plays a role in maintaining the pH and ionic balance of blood by selectively secreting H+ and K+ ions.
Mechanism of Concentration of Filterate
Mammals have the unique ability to produce highly concentrated urine, a process significantly facilitated by Henle’s loop and the vasa recta within the nephron.
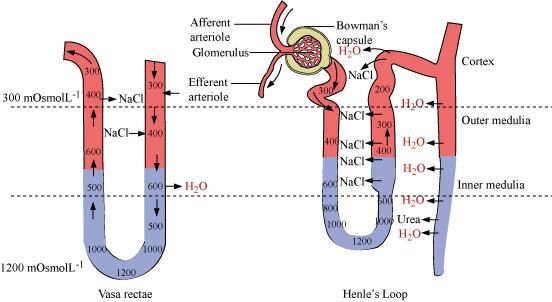 Counter Current Mechanism
Counter Current Mechanism
Counter Current Mechanism
- Henle’s Loop. The flow of filtrate in the two limbs of Henle’s loop is in opposite directions, creating a counter current. This mechanism is crucial for establishing a concentration gradient.
- Vasa Recta. Similarly, the blood flow through the two limbs of the vasa recta also follows a counter current pattern. This alignment, along with the proximity between Henle’s loop and vasa recta, enhances the counter current mechanism.
- Osmolarity Gradient. The counter current flow in both Henle’s loop and vasa recta helps maintain an increasing osmolarity gradient from the cortex (about 300 mOsmol/L. to the inner medulla (up to 1200 mOsmol/L ). This gradient is primarily due to the transport of NaCl and urea.
- Transport of NaCl. NaCl is transported by the ascending limb of Henle’s loop and exchanged with the descending limb of vasa recta. NaCl is then returned to the interstitium by the ascending portion of vasa recta.
- Transport of Urea. Small amounts of urea enter the thin segment of the ascending limb of Henle’s loop and are transported back to the interstitium by the collecting tubule.
- Counter Current Mechanism. The coordinated transport of these substances by Henle’s loop and vasa recta is known as the counter current mechanism. This process is vital for maintaining the concentration gradient in the medullary interstitium.
- Filtrate Concentration. The presence of this interstitial gradient allows for the easy passage of water from the collecting tubule, leading to the concentration of filtrate (urine). Human kidneys are capable of producing urine that is nearly four times more concentrated than the initial filtrate.
|
150 videos|399 docs|136 tests
|
FAQs on Mechanism of Urine Formation & Concentration of Filterate - Biology Class 11 - NEET
| 1. What are the three main steps involved in urine formation? |  |
| 2. How does glomerular filtration work in the kidneys? |  |
| 3. What substances are primarily reabsorbed during the reabsorption phase of urine formation? |  |
| 4. What role does secretion play in urine formation? |  |
| 5. How is the concentration of urine determined, and what factors influence it? |  |