NEET PG Exam > NEET PG Tests > Test: Epilepsy- 2 - NEET PG MCQ
Test: Epilepsy- 2 - NEET PG MCQ
Test Description
15 Questions MCQ Test - Test: Epilepsy- 2
Test: Epilepsy- 2 for NEET PG 2025 is part of NEET PG preparation. The Test: Epilepsy- 2 questions and answers have been prepared
according to the NEET PG exam syllabus.The Test: Epilepsy- 2 MCQs are made for NEET PG 2025 Exam.
Find important definitions, questions, notes, meanings, examples, exercises, MCQs and online tests for Test: Epilepsy- 2 below.
Solutions of Test: Epilepsy- 2 questions in English are available as part of our course for NEET PG & Test: Epilepsy- 2 solutions in
Hindi for NEET PG course.
Download more important topics, notes, lectures and mock test series for NEET PG Exam by signing up for free. Attempt Test: Epilepsy- 2 | 15 questions in 15 minutes | Mock test for NEET PG preparation | Free important questions MCQ to study for NEET PG Exam | Download free PDF with solutions
Test: Epilepsy- 2 - Question 1
In Juvenile myoclonic epilepsy (JME), most common presentation is? (AIIMS May 2013)
Detailed Solution for Test: Epilepsy- 2 - Question 1
Test: Epilepsy- 2 - Question 2
New anti-epileptic drug for Lennox Gastaut syndrome is: (AIIMS Nov 2012)
Detailed Solution for Test: Epilepsy- 2 - Question 2
Test: Epilepsy- 2 - Question 3
A pregnant lady is a known case of juvenile myoclonic epilepsy and is receiving sodium valproate. Which of the following drugs is best suited after valproate for management of this patient. (AIIMS May 2013)
Detailed Solution for Test: Epilepsy- 2 - Question 3
Test: Epilepsy- 2 - Question 4
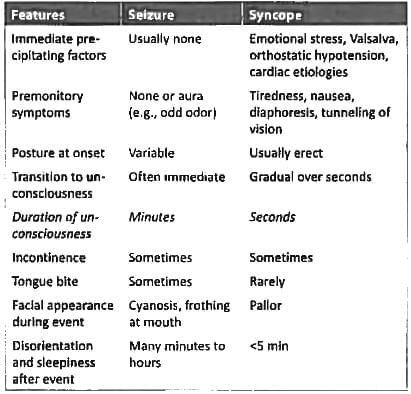
Which can differentiate between seizures and syncope? (AIIMS May 2013)
Detailed Solution for Test: Epilepsy- 2 - Question 4
Test: Epilepsy- 2 - Question 5
A neurosurgeon in parent teacher meeting saw a child with precocious puberty and uncontrollable laughing. He suggested the parent of child to get a MRI done to evaluate for the possibility of: (AIIMS Nov 2012)
Detailed Solution for Test: Epilepsy- 2 - Question 5
Test: Epilepsy- 2 - Question 6
Most common electrolyte abnormality causing seizures in hospitalized patients is: (Recent Pattern 2014/15)
Detailed Solution for Test: Epilepsy- 2 - Question 6
Detailed Solution for Test: Epilepsy- 2 - Question 7
Test: Epilepsy- 2 - Question 8
EEG showing <3hz polyspike activity is seen in: (Recent Pattern 2014/15)
Detailed Solution for Test: Epilepsy- 2 - Question 8
Detailed Solution for Test: Epilepsy- 2 - Question 9
Test: Epilepsy- 2 - Question 10
Periodic lateralized slowing on EEG is seen in: (Recent Pattern 2014/15)
Detailed Solution for Test: Epilepsy- 2 - Question 10
Test: Epilepsy- 2 - Question 11
Atypical febrile seizures are associated with: (Recent Pattern 2014/I5)
Detailed Solution for Test: Epilepsy- 2 - Question 11
Detailed Solution for Test: Epilepsy- 2 - Question 12
Test: Epilepsy- 2 - Question 13
Best drug for photosensitive epilepsy: (Recent Pattern 2014/15)
Detailed Solution for Test: Epilepsy- 2 - Question 13
Test: Epilepsy- 2 - Question 14
6 year old child with abnormal twitching of the face during sleep noticed by mother. EEG shows spikes over centro-temporal area. Diagnosis: (Recent Pattern 2014/15)
Detailed Solution for Test: Epilepsy- 2 - Question 14
Test: Epilepsy- 2 - Question 15
A 29-year old, 4-month pregnant primigravida has history of juvenile myoclonic epilepsy. She has been regularly taking sodium valproate and now seeking an opinion for her antiepileptic regimen. What would you suggest her? (AIIMS May 2012)
Detailed Solution for Test: Epilepsy- 2 - Question 15
Information about Test: Epilepsy- 2 Page
In this test you can find the Exam questions for Test: Epilepsy- 2 solved & explained in the simplest way possible.
Besides giving Questions and answers for Test: Epilepsy- 2, EduRev gives you an ample number of Online tests for practice
Download as PDF