Test: Anemia and RBC Defects - NEET PG MCQ
30 Questions MCQ Test - Test: Anemia and RBC Defects
A 25-year-old female presents to your OPD 1 year postpartum. She was treated for iron deficiency anemia when she was pregnant. Now she is pale and haemoglobin value is 5 gm%. Her reticulocyte count is 9%. Calculate her corrected reticulocyte count. (AIIMS May 2017)
All are causes of Coombs positive haemolytic anaemia except? (AIIMS May 2016)
Severe aplastic anemia is defined as bone marrow cellularity less than _____? (Recent Question 2016-17)
All are essential for diagnosis of Aplastic anemia except? (Recent Question 2016-17)
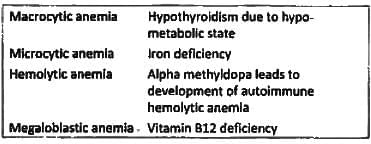
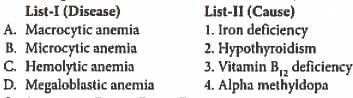
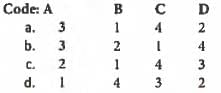
Match List-I with List-II and select the correct answer using the code given below the lists: (UPSC 2015)
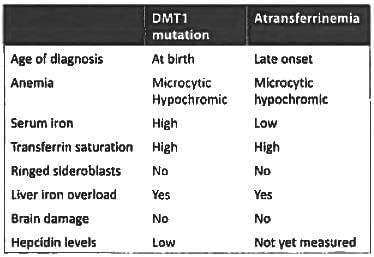
Which one of the following is NOT associated with microcytic hypochromic anemia? (APPG 2015)
All of the following cause microcytic hypochronic anemia, except? (Bihar PG 2015)
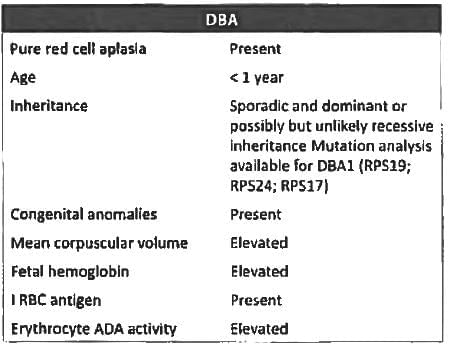
Diamond Blackfann anaemia is associated with? (JIPMER Nov 2015)
A 45-year-old lady diagnosed to have anemia Hb-7.8, MCV = 70 and serum ferritin = 8 ng/dl. After 1 month of iron therapy with adequate dose Hemoglobin is still 8 gm%. What is the most probable cause for treatment failure is? (JIPMER Nov 2014)
In cobalamin deficiency which is not seen? (Recent Question 2015-I6)
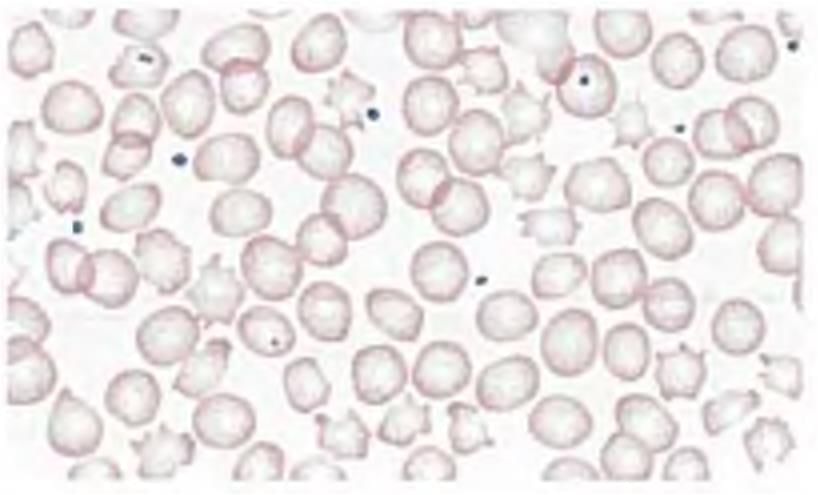
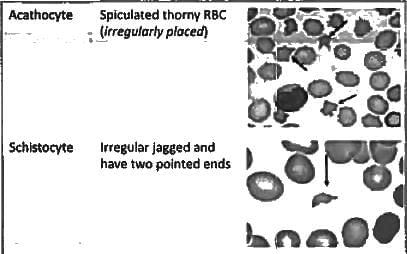
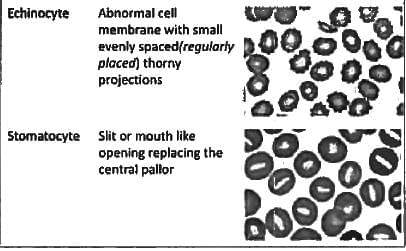
Poikilocytosis and anisocytosis is seen in? (Recent Question 2015-16)
Blood transfusion associated acute lung injury occurs due to? (Recent Question 2015-16)
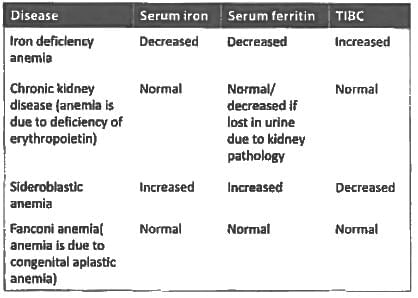
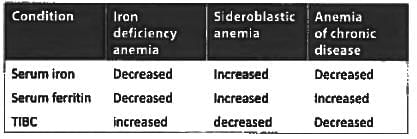
Low serum iron and low serum ferritin is seen in: (Recent Question 2015-16)
All are true about cross-matching of blood except: (Recent Question 2015-16)
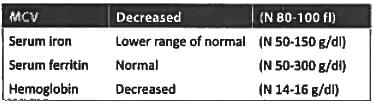
All the following are suggestive of iron-deficiency anemia except: (Recent Pattern 2014-15)
Hemolytic anemia are associated with all of the following, except: (Recent Pattern 2014-15)
A patient with microcytic hypochromic anemia, Hb-9%, serum iron is 20 g/dl, ferritin level 800 ng/ ml, transferrin percentage saturation is 64. What is possible diagnosis: (Recent Pattern 2014-15)
Seen in chronic inflammatory anemia is: (Recent Pattern 2014-15)
Reticulocyte count in Hemolytic jaundice is greater than? (Recent Pattern 2014-15)
Coombs negative hemolytic anemia is seen in: (Recent Pattern 2014-15)
Coomb's positive hemolytic anemia associated with: (Recent Pattern 2014-15)
A patient with previously normal hemoglobin suffered a sudden massive acute hemorrhage. He is most likely to show all of the following except: (Recent Pattern 2014-15)
Spur cell anemia is seen in: (Recent Pattern 2014-15)
Low serum haptogloblin in hemolysis is masked by: (Recent Pattern 2014-15)
Which causes aplastic anemia? (Recent Pattern 2014-15)
A young female has the following lab values: Hemoglobin = 9.8 gm%, MCV = 70 serum iron = 60, serum ferritin = 100, the diagnosis is: (Recent Pattern 2014-15)
Warm-antibody immune-hemolytic anemia is seen in all except: (Recent Pattern 2014-I5)
Anemia of chronic disease is associated with: (Recent Pattern 2014-15)
Which of the following causes of Anemia is associated with a Hypoplastic marrow? (Recent Pattern 2014-15)