Neuroanatomy - 2 Chapter Notes | Anatomy - NEET PG PDF Download
Cerebrospinal Fluid (CSF) and Ventricles
- Cerebrospinal Fluid (CSF) is a clear fluid derived from blood, produced in the choroid plexuses within the brain's ventricles.
- Initially, CSF comes from amniotic fluid and is subsequently produced by the choroid plexus, primarily in the lateral ventricles, with smaller amounts generated in the third and fourth ventricles.
- CSF flows from the lateral ventricle to the third ventricle through the foramen of Monro, then travels through the aqueduct of Sylvius into the fourth ventricle, and finally enters the central canal.
- From the fourth ventricle, CSF exits the ventricular space via three openings (the midline Magendie and two lateral Luschka) into the subarachnoid space.
- CSF is absorbed from the subarachnoid space through the arachnoid villi (or granulations), which extend into the dural venous sinuses (such as the superior sagittal sinus).
- Dural venous sinuses are large vessels situated within the dura mater that collect used blood from the brain, receiving blood from various veins in the brain.
- The primary route for lymphatic CSF absorption is along the olfactory nerve, although other nerves can also transport CSF outside the skull. Tracers placed in the CSF system have demonstrated that they can exit the skull along nearly all cranial nerves, including the optic, trigeminal, vestibulo-cochlear, vagus, and hypoglossal nerves.
- In adults, the total volume of CSF ranges from 140 to 270 mL, with the volume of the ventricles being approximately 25 mL. CSF is produced at a rate of 0.2–0.7 mL per minute (or 600–700 mL per day), resulting in the entire CSF volume being replaced about four times each day.
Circulation and Absorption of Cerebrospinal Fluid (CSF)
- CSF Production and Flow: CSF is produced in the lateral ventricles. From there, it flows through the interventricular foramen of Monro into the third ventricle, located centrally in the brain.
- Passage to the Fourth Ventricle: From the third ventricle, CSF passes through the cerebral aqueduct of Sylvius to reach the fourth ventricle.
- Entry into Sub-Arachnoid Space: CSF then moves from the fourth ventricle into the sub-arachnoid space through foramina in the roof of the fourth ventricle (Magendie and Luschka).
- Distribution over the Cerebrum: CSF circulates over the inferior and superolateral surfaces of the cerebrum.
- Absorption: CSF is absorbed through arachnoid villi and granulations into the dural venous sinus, particularly the superior sagittal sinus.
Formation of the Choroid Plexus: The choroid plexus forms when the vascular pia mater and the ependyma come together closely without any nervous tissue in between. The vascular layer folds into the ventricular cavity, creating small, villous projections covered by cuboidal epithelium from the ependyma. These cuboidal cells have numerous microvilli on their ventricular surfaces.

- Hydrocephalus refers to the enlargement of the brain's ventricular system caused by either an excess production of cerebrospinal fluid (CSF) or a blockage in the pathways through which CSF flows.
- Non-communicating hydrocephalus occurs when there are obstructions within the ventricles, such as congenital aqueductal stenosis, preventing the normal flow of CSF.
- Communicating hydrocephalus takes place when there is a blockage distal to the ventricles, for instance, due to adhesions following tuberculous meningitis, allowing CSF to accumulate.
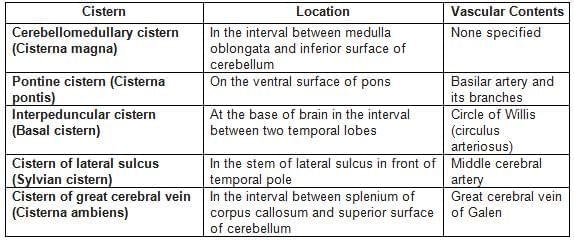
Cerebrospinal Fluid Cisterns of the Brain
Location and vascular contents of various cisterns of the brain.
Lateral Ventricles
Each cerebral hemisphere contains a C-shaped lateral ventricle, lined with ependyma, connecting to the third ventricle via the interventricular foramen (of Monro).
Structure: Comprises a central body and three horns (anterior, posterior, inferior).
- Body: Located in the medial frontal and parietal lobes.
- Floor (lateral to medial): Caudate nucleus body, stria terminalis, thalamostriate vein, thalamus.
- Roof: Corpus callosum.
- Medial wall: Septum pellucidum.
- Anterior (Frontal) Horn: Positioned in the frontal lobe, anterior to the interventricular foramen.
- Roof: Corpus callosum body.
- Floor: Corpus callosum rostrum.
- Anterior wall: Corpus callosum genu.
- Medial wall: Septum pellucidum.
- Lateral wall: Caudate nucleus head.
- Posterior (Occipital) Horn: Found in parietal and occipital lobes.
- Medial wall: Upper part formed by the bulb of the posterior horn (forceps major of corpus callosum); lower part by calcar avis (calcarine sulcus).
- Roof, lateral wall, floor: Tapetum of corpus callosum.
- Inferior (Temporal) Horn: Largest horn, located in the medial temporal lobe.
- Floor: Hippocampus (medial), collateral eminence (lateral).
- Roof: Tail of caudate nucleus and stria terminalis (medial), tapetum of corpus callosum (lateral).
- Trigone (Atrium): Junction of the body, posterior, and inferior horns.
Third Ventricle
- A midline ventricle in the diencephalon, situated between the thalami.
- Lateral walls: Thalamus and hypothalamus.
- Anterior wall: Lamina terminalis.
- Floor: Anteriorly formed by hypothalamic structures; includes the infundibular recess (extending into the pituitary stalk), tuber cinereum, and mammillary bodies.
- Posterior wall: Pineal gland.
- Roof: Ependyma lining the tela choroidea.
- Circumventricular Organs: Specialized areas with tanycytes or modified cells, including the subfornical organ, organum vasculosum (lamina terminalis), subcommissural organ, and linings of pineal, suprapineal, and infundibular recesses.
Fourth Ventricle
- Located in the pons and upper medulla.
- Roof: Formed by the cerebellum (superior and inferior medullary vela).
- Floor: Rhomboid fossa, containing:
- Facial colliculus: Elevation from facial nerve axons looping around the abducens nucleus (internal genu) in the lower pons; lesions cause ipsilateral facial paralysis and unopposed medial eye deviation.
- Obex: Caudal tip, marking the foramen magnum level and medulla-spinal cord division.
- Median sulcus: Divides floor into right and left halves, extending from cerebral aqueduct to spinal cord central canal.
- Stria medullaris: Fibers from arcuate nuclei crossing the floor to the inferior cerebellar peduncle.
- Medial eminence: Elevations beside the median sulcus, bounded by sulcus limitans.
- Sulcus limitans: Separates alar and basal plates; widens into superior fovea (with locus ceruleus, a gray area with norepinephrine-rich neurons containing melanin, termed substantia ferruginea) and inferior fovea.
- Vestibular area: Over vestibular nuclei, lateral to sulcus limitans.
- Vagal trigone: Overlies dorsal motor nucleus of vagus in inferior fovea.
- Hypoglossal trigone: Elevation over hypoglossal nerve nucleus in inferior recess.
Additional Notes
- CSF Flow: Exits the fourth ventricle via one median foramen (Magendie) and two lateral foramina (Luschka) into the subarachnoid space.
- Arachnoid Villi: Protrude mainly into the superior sagittal sinus for CSF absorption.
- Key Features:
- Third ventricle is in the diencephalon.
- Cerebral aqueduct (Sylvius) lies in the mesencephalon.
- Ventricles are lined by ciliated cuboidal/columnar ependymocytes.
- Lateral ventricle connects to third ventricle via foramen of Monro.
- Pineal gland forms the posterior boundary of the third ventricle.
- Foramen of Magendie is the central opening of the fourth ventricle.
- Facial colliculus is in the pons.
Cerebrum
The cerebrum is the largest part of the brain and is responsible for managing various functions such as emotions, personality, hearing, vision, and voluntary actions.
It consists of two cerebral hemispheres, each made up of an outer layer known as the cortex, which is grey matter, and inner regions of axons, which is white matter.
The cerebral cortex is folded into ridges, known as gyri, and furrows, known as sulci, to enhance the surface area. The two hemispheres are divided by a deep groove called the longitudinal fissure.
Lobes of the Cerebral Hemispheres
- Frontal: Involved in reasoning, planning, problem-solving, emotional regulation, and voluntary movement.
- Parietal: Processes sensory information such as touch, temperature, and pain; involved in spatial awareness and perception.
- Occipital: Responsible for visual processing, including the interpretation of visual stimuli such as color, shape, and motion.
- Temporal: Involved in auditory processing, memory, language comprehension, and emotional responses.
- Insular: Plays a role in self-awareness, emotional regulation, and the perception of bodily sensations.
- Limbic: Involved in emotion, memory, and motivation; includes structures such as the hippocampus and amygdala.
The dominant hemisphere is responsible for managing propositional language, which includes grammar, speech, and calculations. In 95% of individuals, the left hemisphere is the dominant one. The non-dominant hemisphere mainly handles spatial awareness and nonverbal ideation, such as music and poetry.
Cerebral Cortex The cerebral cortex is made up of the neocortex, which constitutes 90% of the cortex, and the allocortex, which makes up 10%. The neocortex has six layers, while the allocortex consists of three layers. The allocortex includes the archicortex, which contains the hippocampus and the dentate gyrus, and the paleocortex, which houses the olfactory cortex.
Six Layers of the Neocortex
- Layer I: Molecular Layer
- Layer II: External Granular Layer
- Layer III: External Pyramidal Layer. Produces association and commissural fibers and is a key source of corticocortical fibers.
- Layer IV: Internal Granular Layer. Receives thalamocortical fibers from specific thalamic nuclei. In the visual cortex (Brodmann’s area 17), this layer receives input from the lateral geniculate body.
- Layer V: Internal Pyramidal Layer. Gives rise to corticobulbar, corticospinal, and corticostriatal fibers. It contains the giant pyramidal cells of Betz, which are found only in the motor cortex (Brodmann’s area 4).
- Layer VI: Multiform Layer. The main source of corticothalamic fibers and produces projection, commissural, and association fibers.
Sulci in the Cerebrum
- The Central Sulcus, also known as the sulcus of Rolando, begins approximately 1 cm behind the center of the brain, cutting into the superomedial edge of the hemisphere.
- It extends at a 70° angle downwards and forwards, terminating just above the lateral sulcus.
- The upper end of this sulcus extends onto the medial surface of the hemisphere.
- The central sulcus serves as a boundary between the frontal motor area in the front and the parietal sensory area at the back.
- The Lateral Sulcus, also known as the sulcus of Sylvius, originates as a deep groove on the underside of the cerebral hemisphere, at the anterior perforated substance, which contains small openings for blood vessels.
- It extends outward between the temporal pole and the posterior part of the orbital surface of the hemisphere.
- The lateral sulcus continues backward and slightly upward across the side surface of the hemisphere, ending in the inferior parietal lobule with a turned-up end.
- The Calcarine Sulcus forms on the medial surface of the cerebral hemisphere.
- It begins just below the rear end of the splenium of the corpus callosum and follows an arched path, curving upwards toward the occipital pole.
- This sulcus also extends onto the superolateral surface of the hemisphere.
Types of Sulci in the Brain
- Axial Sulci. These sulci develop along the long axis of rapidly growing, uniform areas in the brain. They appear as longitudinal folds. A notable example is the back part of the calcarine sulcus located in the visual cortex.
- Central Sulcus. This sulcus plays a crucial role in separating the frontal motor cortex from the parietal sensory cortex, marking an important division in the brain's functional areas.
- Operculated Sulcus. While similar to a limiting sulcus in that it separates different areas both structurally and functionally, the operculated sulcus does so at the lip rather than at the base. This sulcus often contains a third functional area within its walls and floor. An example is the lunate sulcus, which separates the striate and peristriate areas at the surface and houses the peristriate area within its walls.
- Complete Sulcus. These sulci are deep enough to create a noticeable bump in the wall of a ventricle. For instance, the collateral sulcus leads to the formation of a collateral eminence in the inferior horn of the lateral ventricle. Similarly, the front part of the calcarine sulcus causes the formation of calcar avis in the medial wall of the occipital horn of the lateral ventricle.
- Insula. The insula is a region of the cerebral cortex located deep within the floor of the lateral sulcus. During development, as nearby cortical areas expand, the insula becomes concealed and is visible only by pulling apart the edges of the lateral sulcus. The insula has a triangular shape and is entirely surrounded by the circular sulcus, except at the front bottom point known as the limen insulae.
- Hippocampus. Situated in the medial temporal lobe, the hippocampus is crucial for memory formation. It is located adjacent to the inferior horn of the lateral ventricle.
- Lunate Sulcus. This sulcus is classified as an operculated sulcus.
Brodmann Areas
Brodmann areas are regions of the cerebral cortex classified based on their cell structure, which is closely associated with specific brain functions. There are a total of 52 areas, which are further divided into 11 histological categories.
Primary Somatosensory Cortex
- Areas 1, 2, and 3, located in the postcentral gyri, constitute the primary somatosensory cortex.
- Area 5 functions as the somatosensory association cortex, integrating sensory information from different modalities.
Primary Motor Cortex
- Area 4, situated in the precentral gyrus, is responsible for voluntary motor control and is known as the primary motor cortex.
- Area 6 includes the premotor cortex and the supplementary motor cortex, both of which are involved in planning and coordinating movements.
Visual Cortex
- Area 17, located in the occipital cortex, is the primary visual area (V1), responsible for initial processing of visual information.
- Area 18 is known as the secondary visual cortex (V2), which further processes visual stimuli.
- Area 19 is referred to as the associative visual cortex (V3, V4, V5), involved in higher-order visual processing and interpretation.
Auditory Cortex
- The auditory cortex, comprising areas 41 and 42, is located in the anterior part of the superior temporal gyri, specifically in Heschl’s gyrus. This area is crucial for processing auditory information.
Wernicke’s Area
- Wernicke’s sensory speech area, located in area 22 of the posterior superior temporal gyrus, plays a vital role in language comprehension.
- The precise boundaries of Wernicke’s area are not well-defined; some researchers include areas 22 and 37, which are involved in visual and auditory processing as well as language functions.
- Areas 39 (angular gyrus) and 40 (supramarginal gyrus) are also mentioned by some authors as part of Wernicke’s area.
- This region is essential for understanding language, but stimulation can disrupt speech production.
Broca’s Area
- Broca’s motor speech area is situated in the inferior frontal gyrus, covering left Brodmann areas 44 (pars opercularis) and 45 (pars triangularis).
- This area is responsible for planning and coordinating speech movements and is crucial for language production.
Frontal Eye Field
- Area 8 is located in the middle frontal gyrus and is involved in controlling horizontal eye movements to the opposite side.
- A lesion in this area can impair voluntary eye movements towards the affected side, causing the eyes to drift slowly towards the side of the lesion.
Other Areas
- Area 43 is known as the primary gustatory cortex, responsible for processing taste information.
- Areas 13 and 14 are referred to as the insular cortices, involved in various functions including sensory processing and autonomic regulation.
- The paracentral lobule, located near the midline, extends from the precentral and postcentral gyri and is involved in controlling motor and sensory functions of the opposite lower limb and perineal region.
- This area also plays a role in bladder and bowel control, including defecation and urination.
Homunculus
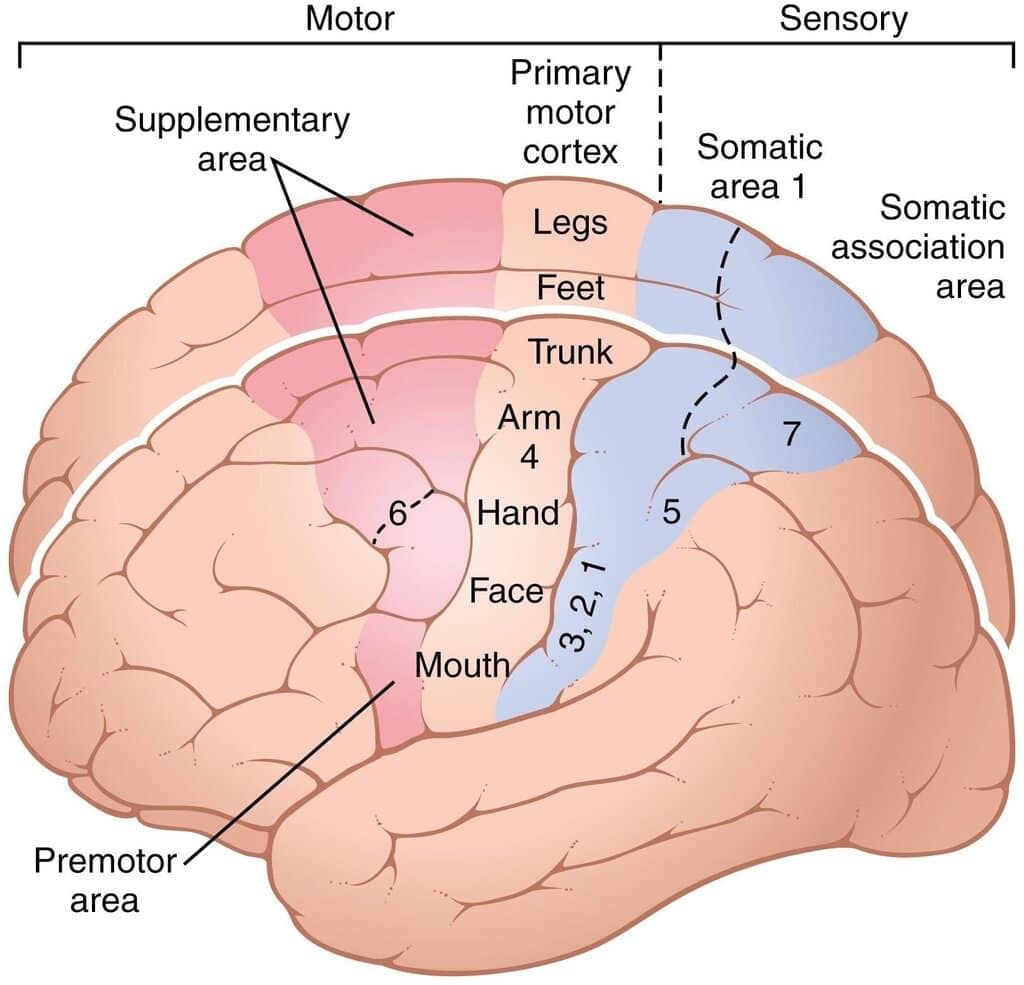
Motor and Somatosensory Areas of the Cerebral Cortex: The motor and somatosensory functional areas of the cerebral cortex are crucial for movement and sensation. These areas are identified by their Brodmann numbers, which are unique identifiers for different regions of the brain.
Sensory and Motor Homunculi: (A) Sensory Homunculus: This represents the sensory areas of the body as mapped onto the postcentral gyrus of the brain. It shows how different parts of the body are represented in the brain for sensory processing. (B) Motor Homunculus: This represents the motor areas of the body as mapped onto the precentral gyrus. It illustrates how different parts of the body are controlled by the brain for voluntary movements.
Language Pathway
Processing a Written Word: When you see a word, the visual information is processed by the brain in a specific sequence:
- Step 1: Visual Processing. The visual image of the word is initially processed in the visual cortex, located in area 17 of the brain.
- Step 2: Association Areas. From there, the information is sent to the visual association areas, specifically areas 18 and 19, for further processing.
- Step 3: Angular Gyrus. The processed visual information is then transferred to the angular gyrus, located in area 39. This area plays a crucial role in integrating visual and auditory information.
- Step 4: Wernicke's Area. In the angular gyrus, the visual information is converted into its auditory form and sent to Wernicke's area, situated in area 22 of the brain. Wernicke's area is responsible for language comprehension and processing the auditory form of the word.
- Step 5: Arcuate Fasciculus. The arcuate fasciculus, a bundle of nerve fibers, carries the processed information from Wernicke's area to Broca’s area, located in areas 44 and 45 of the brain.
- Step 6: Broca’s Area. Broca’s area is responsible for speech production and language processing. It controls the muscle movements necessary for speech, which are mapped onto the precentral gyrus, area 4 of the brain.
Clinical Correlations
- Dysphasia: Dysphasia is a language disorder that can arise from damage to specific areas of the brain involved in language processing and production. Depending on which area is affected, different types of dysphasia can occur.
- Broca’s Expressive Aphasia: This type of dysphasia occurs when Broca’s area, responsible for speech production, is damaged. Patients with Broca’s expressive aphasia have difficulty planning and coordinating the movements needed for speech. Their speech is often hesitant and consists of short, fragmented phrases rather than complete sentences. While they generally understand language well, they are aware of their speech difficulties and may become frustrated by their inability to communicate effectively.
- Wernicke’s Receptive Aphasia: Wernicke’s receptive aphasia occurs when Wernicke's area, which is responsible for language comprehension, is damaged. Patients with this condition have difficulty understanding spoken and written language. Their speech may be fluent but lacks meaning, often consisting of irrelevant or nonsensical sentences. Unlike patients with Broca’s aphasia, those with Wernicke’s aphasia are often unaware of their errors and the lack of coherence in their speech.
- Conduction Aphasia: Conduction aphasia results from a lesion in the arcuate fasciculus, the neural pathway connecting Wernicke's area and Broca’s area. Patients with conduction aphasia experience difficulties in naming objects and repeating words or phrases. However, their ability to understand language and their speech fluency remain intact. They are aware of their mistakes but struggle to correct them, leading to frustrations in communication.
Basal Ganglia
Brain Parts Involved in Controlling Voluntary Movements:
- Voluntary movement begins in the cerebral cortical association areas.
- The cerebral cortex, basal ganglia, and cerebellum collaborate to plan movements.
- When the cortex initiates a movement, the signal travels through the pyramidal tract, which includes the corticospinal and corticobulbar tracts, to reach the motor neurons.
- The cerebellum provides feedback to help adjust and smooth out these movements.
- Basal ganglia play a crucial role in starting and stopping voluntary movements and in inhibiting unwanted movements.
- The basal ganglia consist of several nuclei, including:
- Caudate nucleus
- Putamen
- Globus pallidus
- These are deep within the cerebrum. The basal ganglia also include two functional nuclei:
- Substantia nigra, located in the midbrain
- Subthalamic nucleus, located in the diencephalon
- The amygdaloid nucleus is primarily associated with the limbic system. The function of the claustrum within the basal ganglia is not well understood.
Connections within the Basal Ganglia
- The striatum receives important input from three main sources: the thalamus, neocortex, and substantia nigra.
- The striatum sends signals to two key areas: the globus pallidus and substantia nigra.
- The globus pallidus serves as the primary output center for the striatal system, relaying information to the thalamus and subthalamic nucleus.
- The substantia nigra is involved in movement control and reward processes; it also sends projections to the thalamus.
- The striatal motor system operates through the pyramidal system, which encompasses the corticobulbar and corticospinal tracts.
Functions of the Basal Ganglia
- The basal ganglia are crucial for planning and programming movements, transforming abstract ideas into voluntary actions.
- They play a significant role in initiating and executing voluntary motor activities, especially those driven by will.
- Additionally, the basal ganglia are involved in automatic and habitual postures, as well as reflex actions, such as the natural arm swing during walking.
- The basal ganglia also regulate muscle tone, ensuring smooth voluntary movements and minimizing unwanted muscle activity.
- They help determine the speed and magnitude of movements, as well as control movements associated with emotional expressions and reflex muscle activities.
- Key components of the basal ganglia include the globus pallidus and putamen, which are involved in various motor control functions.
- The amygdaloid nucleus is also part of the basal ganglia and contributes to their functions.
Internal Capsule
The internal capsule is a structure in the lower middle part of the cerebral hemisphere, consisting of a bundle of axons (white matter). It plays a crucial role in connecting different parts of the brain.
Inside the internal capsule, there are both ascending and descending projection fibers that link higher brain areas with lower ones and vice versa. It acts as a separator, distinguishing the caudate nucleus and the thalamus from the lentiform nucleus, which includes the putamen and globus pallidus.
When viewed in cross-section, the internal capsule appears V-shaped, comprising an anterior limb, a posterior limb, and a bend called the genu.
The anterior limb is situated between the head of the caudate nucleus and the lentiform nucleus. It carries fibers connecting the cerebral cortex with the thalamus and the basal ganglia.
- The genu contains sensory and motor fibers for the head.
- The posterior limb is divided into three parts:
- Front two-thirds. Carries sensory and motor fibers for the body, with upper body fibers more towards the front and lower body fibers towards the back.
- Back one-third. Carries sensory fibers, including those for audio-visual pathways.
The retrolenticular portion, located behind the lentiform nucleus, contains the optic radiation (geniculo-calcarine tract), which transmits visual information from the lateral geniculate body to the occipital visual cortex (calcarine fissure).
The sublentiform portion, situated beneath the lentiform nucleus, carries the auditory pathway from the medial geniculate nucleus to the primary auditory cortex (superior temporal gyrus).
Fiber Types in Different Parts of the Internal Capsule
1. Anterior Limb.
Motor Fibers:
- Corticopontine fibers
- Corticobulbar (corticobulbar) and corticospinal fibers for the head and neck.
- Sensory Fibers:Superior Thalamic Radiation (anterior part only)
2. Posterior Limb.
Motor Fibers:
- Corticopontine fibers
- Corticospinal fibers for the upper limb, trunk, and lower limb.
- Corticorubral (extrapyramidal) fibers.
- Sensory Fibers:Posterior Thalamic Radiation (optic radiation)
3. Retrolentiform Part.
- Sensory Fibers:
- Posterior Thalamic Radiation (optic radiation)
4. Sublentiform Part.
- Sensory Fibers:
- Inferior Thalamic Radiation (auditory radiation)
The pyramidal tract, comprising the corticospinal and corticonuclear tracts, constitutes a significant portion of the internal capsule. It transmits signals from upper motor neurons in the cerebral cortex to lower motor neurons in the brainstem and spinal cord, regulating skeletal muscle activity.
Above the basal nuclei, the pyramidal tract is referred to as the corona radiata, while below the basal nuclei, it is known as the crus cerebri, part of the cerebral peduncle.
Within the genu of the internal capsule, the corticonuclear tracts carry upper motor neuron fibers destined for the skeletal muscles of the head. These fibers cross over and terminate in the motor nuclei of the cranial nerves on the opposite side.
The posterior limb of the internal capsule contains the corticospinal tract, which carries upper motor neuron fibers for the skeletal muscles of the lower body, including the neck, trunk, and limbs.
The trigeminal system transmits sensory fibers from the head, which pass through the genu of the internal capsule. Sensory fibers from the lower body, originating from various tracts such as the dorsal column and spinothalamic tract, also traverse the posterior limb of the internal capsule.
Blood Supply to the Internal Capsule
The internal capsule receives its blood supply from arteries that originate from the circle of Willis and associated vessels. The majority of the internal capsule is supplied by the lateral and medial striate arteries, which branch off from the middle and anterior cerebral arteries.
Main Arteries Supplying the Internal Capsule:
- Middle Cerebral Artery: This is the primary source of blood supply.
- Anterior Cerebral Artery: This includes the recurrent branch of Heubner.
- Anterior Choroidal Artery: This artery branches from the internal carotid artery.
In addition to these main arteries, the internal capsule also receives branches from the internal carotid artery, posterior communicating artery, and posterior cerebral artery.
Segmentation of Blood Supply: The blood supply to the internal capsule is divided into two main sections: superior (dorsal) and inferior (ventral).
Superior (Dorsal) Part: This section includes the upper part of the anterior limb, genu, and posterior limb, which are supplied by the lenticulo-striate branches of the middle cerebral artery.
Inferior (Ventral) Part: This part includes:
- Anterior Limb: Supplied by the anterior cerebral artery, including the recurrent branch of Heubner.
- Genu: Supplied by the internal carotid artery.
- Posterior Limb: Supplied by the anterior choroidal artery.
Sublentiform and Retrolentiform Areas: These areas are primarily supplied by the anterior choroidal artery.
Clinical Significance:
- Charcot’s Artery of Cerebral Hemorrhage: This is a notable striate branch of the middle cerebral artery.
- Ischemic Damage: Damage to the internal capsule due to ischemia results in loss of sensation and movement (hypoesthesia and hemiparesis with the Babinski sign) on the opposite side of the body.
- Specific Lesion Effects: Lesions in different areas of the internal capsule lead to specific deficits:
- Genu: Causes loss of sensation and movement in the head area.
- Anterior Two-Thirds of the Posterior Limb: Causes loss of sensation and movement in the body, including the neck, trunk, and limbs.
- Posterior Limb (Last Third): Causes visual and auditory disturbances, such as homonymous hemianopia.
Corticonuclear Tract: This tract passes through the genu of the internal capsule.
Sublentiform Part and Acoustic Radiation: The sublentiform part of the internal capsule is associated with the acoustic radiation.
Diencephalon
The diencephalon is a region of the forebrain, also known as the prosencephalon. It includes the thalamus and other related structures. The diencephalon plays a vital role in integrating sensory and motor systems. Within the diencephalon, there is the third ventricle, which is located in the midline. This ventricle is the cavity of the thalamus and lies between the two thalami.
Components of Diencephalon
- Hypothalamus (including the posterior pituitary)
- Epithalamus, which consists of:
- Anterior and posterior paraventricular nuclei
- Medial and lateral habenular nuclei
- Stria medullaris thalami
- Posterior commissure
- Pineal body
- Subthalamus
- Metathalamus (containing the medial and lateral geniculate bodies)
During embryonic development, the diencephalon gives rise to the optic cup, which later develops into the retina and optic nerve.
Thalamus: Overview
The thalamus is a crucial part of the diencephalon and acts as the primary hub for relaying sensory and motor signals to the cerebral cortex. Additionally, it plays a significant role in regulating consciousness, sleep, and alertness.
The two thalami are located on either side of the third ventricle and are connected by a thin band of grey matter called the interthalamic adhesion, which passes through the ventricle.
Thalamic Nuclei
Within the thalamus, there is a ventral posterior (VP) nucleus that is divided into two sections: medial and lateral.
- The Ventral-Posterior-Medial (VPM) nucleus is responsible for receiving sensory input from the head region.
- The Ventral-Posterior-Lateral (VPL) nucleus receives sensory information from the body.
Sensory Pathways to the Thalamus
- Trigeminal Nerve to VPM: The trigeminal nerve (first-order neuron) carries sensory information from the head and transmits it to the VPM nucleus of the thalamus via the trigeminal lemniscus (second-order neuron in the brainstem).
- Thalamocortical Projections: Third-order neurons in the thalamus project sensory information to the parietal sensory cortex (areas 1, 2, 3).
Spinothalamic Tract and Dorsal Column to VPL:
- Spinothalamic Tract: Carries information about pain and temperature from the body to the VPL nucleus.
- Dorsal Column: Transmits information on tactile discrimination and vibration to the VPL nucleus.
Sensory Input to the Thalamus
- The thalamus receives input from all sensory systems except for the olfactory system.
- It connects to the cerebral cortex through the thalamocortical radiations and to the hippocampus via the mammillo-thalamic tract.
- The thalamus also has important connections with the basal nuclei.
Spinothalamic Tract in the Spinal Cord
- The spinothalamic tract in the spinal cord conveys information to the thalamus about crude touch, pressure, pain, and temperature sensations.
Metathalamus
The metathalamus is made up of the medial and lateral geniculate bodies.
Lateral Geniculate Body
- The lateral geniculate body plays a crucial role in the visual pathway.
- It functions as a relay station for visual information.
- This structure receives input from the retina via the optic tract.
- Subsequently, it sends projections to the primary visual cortex, also known as V1.
- The lateral geniculate body is organized into a six-layered structure.
Medial Geniculate Body
- The medial geniculate body is an integral part of the auditory pathway.
- It acts as an auditory relay nucleus, processing auditory information.
- This structure receives auditory input through the brachium of the inferior colliculus.
- From there, it projects to the primary auditory cortex, specifically areas 41 and 42.
Hypothalamus
The hypothalamus is a crucial part of the diencephalon, situated at the lower and lateral aspects of the third ventricle in the brain. Its primary function is to maintain homeostasis by regulating the autonomic nervous system, the endocrine system, and the limbic system.
This section focuses on the various hypothalamic nuclei and their specific roles in the body's regulatory processes.
Connections of the Hypothalamus
- The fornix is composed of five parts: the alveus, fimbria, crus, body, and columns.
- It serves as a connecting pathway between the hippocampal formation and the mammillary nucleus, the anterior nucleus of the thalamus, and the septal area.
- Disruption of specific pathways through bilateral cutting can lead to an acute amnestic syndrome.
- The stria terminalis is a fiber tract that originates from the amygdaloid complex and connects the septal area with the hypothalamus.
- It is located in the sulcus terminalis, which is situated between the caudate nucleus and the thalamus.
- The mammillothalamic tract is a neural pathway that extends from the mammillary nuclei to the anterior nucleus of the thalamus.
- The hypothalamospinal tract contains descending autonomic fibers that influence the preganglionic sympathetic neurons located in the lateral horn cells and the preganglionic neurons of the sacral parasympathetic nucleus within the spinal cord.
- A lesion or damage to this tract may result in Horner syndrome, a condition characterized by a specific set of symptoms including ptosis, miosis, and anhidrosis.
Subthalamus
The subthalamus is a part of the diencephalon located beneath the thalamus. It is situated medial to the internal capsule and dorsolateral to the hypothalamus.
Efferent Connections
The subthalamus sends outgoing connections to several areas, including:
- Striatum (caudate nucleus and putamen) in the telencephalon
- Dorsal thalamus (medial and lateral nuclear groups) in the diencephalon
- Red nucleus and substantia nigra in the mesencephalon
Afferent Connections
It receives incoming connections from the substantia nigra and striatum.
Neuronal Effects
Neurons in the subthalamus produce glutamate, which has an excitatory effect on neurons in the globus pallidus and substantia nigra.
Reticular Nuclei
The reticular nucleus is a thin layer of GABAergic neurons that surrounds the thalamus. It is located between the external medullary lamina and the internal capsule. This nucleus plays a crucial role in regulating thalamic activity.
- Location and Composition. The reticular nucleus is situated around the thalamus, composed of GABAergic neurons, which are inhibitory in nature.
- Inputs. It receives excitatory inputs from both corticothalamic and thalamocortical fibers.
- Outputs. The reticular nucleus sends inhibitory GABAergic fibers to the thalamic nuclei from which it receives input.
- Function. This nucleus modulates thalamic activity by providing inhibitory feedback, thereby playing a critical role in the regulation of sensory information.
- Connectivity. Reticular nuclei have connections within the thalamus and do not project to the cortex.
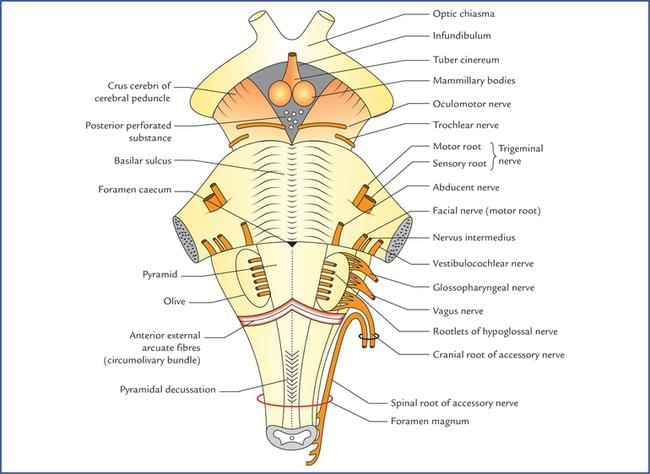
Brainstem
The brainstem is a vital part of the central nervous system, comprising the midbrain, pons, and medulla. It extends from the posterior commissure to the pyramidal decussation and contains the nuclei for cranial nerves III to XII, with the nerve fibers exiting from it.
Several important motor and sensory pathways pass through the brainstem, including:
- Corticospinal tract (motor)
- Dorsal column-medial lemniscal tract
- Spinothalamic tract—spinal lemniscal system
- Trigeminal lemniscus
- Lateral lemniscus (auditory pathway)
The brainstem also houses the reticular formation, which is located at its central core. The brainstem plays a crucial role in regulating various autonomic functions, including:
- Cardiac function (heart rate)
- Respiratory function (breathing)
Additionally, it regulates the central nervous system, maintains consciousness, and controls the sleep cycle. The arterial supply to the brainstem comes from branches of the vertebral arteries and the basilar arteries.
Midbrain
Midbrain (Mesencephalon) Overview
- Structure: The midbrain consists of three regions: the dorsal tectum, intermediate tegmentum, and ventral base.
- Anatomical Boundaries: Extends from the posterior commissure to the superior medullary velum.
- Connections: Linked to the cerebellum via the superior cerebellar peduncle.
- Key Nuclei:
- Oculomotor nucleus located at the superior colliculus level.
- Trochlear nucleus situated at the inferior colliculus level.
- Substantia nigra, the largest midbrain nucleus.
- Functional Centers: Contains a rostral center for vertical conjugate gaze.
- Reticular Formation: Paramedian reticular formation lies along the midline.
- Lemnisci: Four lemnisci (from medial to lateral): medial, trigeminal, spinal, and lateral.
- Ventricle: The cerebral aqueduct of Sylvius, located between the tectum and tegmentum, serves as the midbrain’s ventricle.
Transverse Section of the Midbrain
- Dorsal Structures: Superior and inferior colliculi.
- Tegmentum Structures:
- Oculomotor nucleus
- Medial longitudinal fasciculus
- Red nucleus
- Substantia nigra
- Dentatothalamic tract (crossed)
- Medial lemniscus
- Lateral spinothalamic tract (within the spinal lemniscus)
- Crus Cerebri (Cerebral Peduncle): Contains the corticospinal tract in its middle three-fifths.
Midbrain Syndromes
- Weber Syndrome (Medial Midbrain Syndrome)
- Cause: Occlusion of paramedian branches of the upper basilar and proximal posterior cerebral arteries.
- Ipsilateral Symptoms (Affected Structures):
- "Down and out" eye with dilated, unresponsive pupil and ptosis (oculomotor nerve fibers).
- Eye abduction and depression due to unopposed lateral rectus (CN 6) and superior oblique (CN 4).
- Severe ptosis from levator palpebrae paralysis.
- Fixed, dilated pupil (complete internal ophthalmoplegia).
- Contralateral Symptoms (Affected Structures):
- Weakness of the lower face (CN 7), palate (CN 10), and tongue (CN 12) due to corticobulbar tract involvement in crus cerebri.
- Hemiparesis of trunk and limbs (corticospinal tract in crus cerebri).
- Possible parkinsonism features (substantia nigra).
- Lateral Midbrain Syndrome
- Cause: Occlusion of posterior cerebral artery branches.
- Ipsilateral Symptoms (Affected Structures):
- "Down and out" eye with dilated, unresponsive pupil and ptosis (oculomotor nerve nucleus and fibers).
- Contralateral Symptoms (Affected Structures):
- Hemiataxia, hyperkinesia, and tremors (red nucleus and dentato-rubro-thalamic tract).
- Benedikt Syndrome (Paramedian Midbrain Syndrome)
- Cause: Occlusion of paramedian branches of the posterior cerebral artery.
- Ipsilateral Symptoms (Affected Structures):
- "Down and out" eye with dilated, unresponsive pupil and ptosis (oculomotor nerve fibers).
- Eye abduction and depression due to unopposed lateral rectus (CN 6) and superior oblique (CN 4).
- Severe ptosis from levator palpebrae paralysis.
- Fixed, dilated pupil (complete internal ophthalmoplegia).
- Contralateral Symptoms (Affected Structures):
- Hemiataxia, hyperkinesia, and tremors (red nucleus and dentato-rubro-thalamic tract).
- Loss of proprioception, discriminative touch, and vibration sense (medial lemniscus).
- Parinaud Syndrome (Posterior Midbrain Syndrome)
- Cause: Often due to a pineal tumor.
- Symptoms (Affected Structures):
- Paralysis of upward and downward gaze, pupillary abnormalities, and loss of convergence (superior colliculus and pretectal area lesion).
- Non-communicating hydrocephalus due to compression of the cerebral aqueduct of Sylvius.
|
68 docs|16 tests
|
FAQs on Neuroanatomy - 2 Chapter Notes - Anatomy - NEET PG
| 1. What is the role of cerebrospinal fluid (CSF) in the central nervous system? |  |
| 2. What are the major functions of the thalamus in the brain? |  |
| 3. How does the homunculus represent the human body's sensory and motor functions? |  |
| 4. What is the significance of Brodmann areas in neuroanatomy? |  |
| 5. What are the main components of the basal ganglia and their functions? |  |




















