Neuroanatomy - 4 Chapter Notes | Anatomy - NEET PG PDF Download
Spinothalamic Tract (STT)
The spinothalamic tract is responsible for transmitting different types of sensory information from the body to the brain. It is divided into two main components: the lateral spinothalamic tract and the anterior spinothalamic tract.
Lateral Spinothalamic Tract – Spinal Lemniscal System
- First-order neurons in the dorsal root ganglion send fibers that ascend one or two spinal segments before synapsing in the dorsal horn of the spinal gray matter.
- These neurons synapse with second-order neurons in the posterior horn. The axons of these second-order neurons cross the midline via the anterior white commissure, forming the lateral spinothalamic tract in the spinal cord, which continues as the spinal lemniscus in the brainstem.
- Third-order neurons in the ventral posterolateral (VPL) nucleus of the thalamus project through the posterior limb of the internal capsule to the primary somatosensory cortex (postcentral gyrus, Brodmann areas 1, 2, 3).
- The anterior spinothalamic tract plays a minor role in transmitting light and crude touch and pressure sensations, as well as itch and tickling.
- Its pathway mirrors that of the lateral spinothalamic tract, merging with it at the spinal lemniscus in the brainstem before reaching the thalamus. Some touch sensation axons may join the medial lemniscus en route to the thalamus.
- Ventral corticospinal tract and medial descending brainstem pathways (tectospinal, reticulospinal, and vestibulospinal tracts) regulate proximal muscles and posture.
- Lateral corticospinal and rubrospinal tracts control distal limb muscles for fine motor skills and voluntary movements.
- The posterior column tract does not transmit temperature sensations; these are carried by the lateral spinothalamic tract (AIPG 2008).
- Stereognosis, the ability to recognize an unseen familiar object, is mediated by the dorsal column.
- An anterolateral cordotomy relieves pain in the left leg by interrupting the right lateral spinothalamic tract.
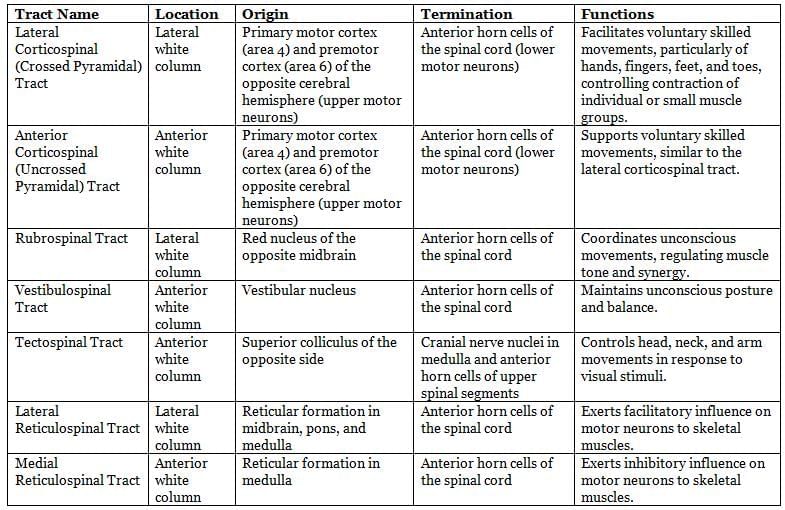
Major descending tracts in the spinal cord.
Pyramidal System
The pyramidal tract is made up of fibers from pyramidal neurons found in layer 5 of the precentral gyrus, premotor areas, and somatic sensory cortex. These fibers travel down through the posterior limb of the internal capsule and the basis pedunculi, cross at the spinomedullary junction, and form the lateral corticospinal tract in the spinal cord's lateral funiculus. They connect to lower motor neurons in the ventral horn or to interneurons.
- Most muscles are controlled by the contralateral motor cortex. However, some muscles, like those in the upper face, those used for chewing, and larynx muscles, are controlled by both sides of the brain.
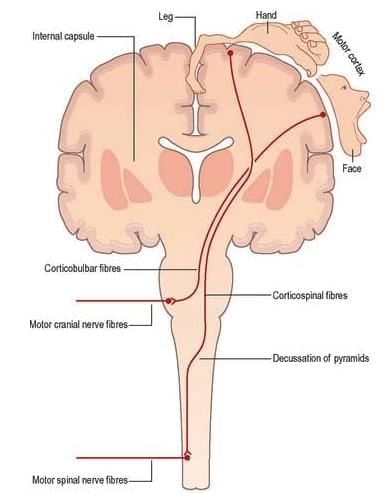
- Damage to the pyramidal tract above the crossing point leads to: spastic paralysis, loss of fine movements, and hyper-reflexia on the opposite side.
- Damage to the corticospinal tract in the spinal cord results in symptoms on the same side of the body.
- Brown-Sequard syndrome occurs with hemisection of the spinal cord, causing weakness or paralysis (hemiplegia. on the same side and loss of sensation (hemianesthesia. on the opposite side.
Autonomic Nervous System
The autonomic nervous system (ANS) is responsible for controlling the involuntary movements of cardiac muscle, smooth muscle, and glands. It is divided into three parts: sympathetic, parasympathetic, and enteric divisions.
The ANS includes both general visceral efferent (GVE) and general visceral afferent (GVA) fibers. The motor part of the ANS consists of two neurons: preganglionic and postganglionic.
Preganglionic Neurons
- Preganglionic neurons have their cell bodies in the central nervous system (CNS), specifically in the brainstem and the lateral grey columns of the spinal cord.
- Their axons are usually finely myelinated, which helps in faster signal transmission.
- These neurons exit the CNS through specific cranial and spinal nerves.
- Preganglionic axons connect to peripheral ganglia, where they synapse with postganglionic neurons.
Postganglionic Neurons
- The axons of postganglionic neurons are typically unmyelinated, which means they do not have the myelin sheath that speeds up transmission.
- There are generally more postganglionic neurons than preganglionic ones.
- One preganglionic neuron can synapse with multiple postganglionic neurons, often ranging from 15 to 20.
- This arrangement allows for a wide distribution of autonomic effects throughout the body.
Location and Distribution
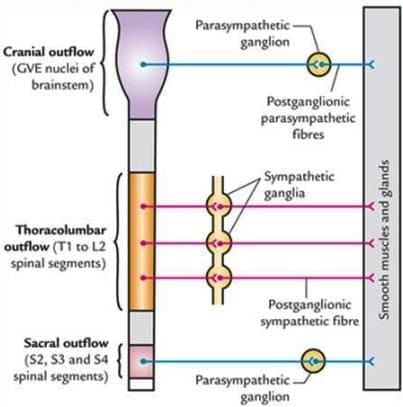
- The sympathetic nervous system originates from the thoracolumbar region of the spinal cord, while the parasympathetic nervous system arises from the craniosacral area.
- Autonomic activity is not solely dependent on the reflex connections of General Visceral Afferent (GVA) pathways. Impulses in these pathways do not always activate General Visceral Efferents (GVEs).
- Peripheral autonomic activity is coordinated at higher levels in the brainstem and cerebrum. This coordination involves various nuclei in the brainstem reticular formation, thalamus, hypothalamus, limbic system, and prefrontal cortex, along with the pathways connecting these areas.
- The parasympathetic system is primarily located in the head, neck, and body cavities. It is not present in the body wall or limbs, except for the erectile tissues of the genitalia.
- Sympathetic fibers are widely distributed throughout the body, particularly to vascularized areas.
Neurotransmitters in the Autonomic Nervous System
In general, neurons involved in the autonomic nervous system use specific neurotransmitters to communicate.
- Preganglionic Neurons: In both the sympathetic and parasympathetic systems, these neurons release acetylcholine (ACh). The receptors on the target cells are nicotinic receptors.
- Postganglionic Neurons:
- Parasympathetic: These neurons also use acetylcholine (ACh), but the receptors on the target cells are muscarinic.
- Sympathetic: Most of these neurons release norepinephrine (NE). However, there are exceptions, such as the neurons that innervate eccrine sweat glands, which use acetylcholine (ACh) instead.
Co-Transmitters in the Autonomic Nervous System
- Sympathetic Nerves: In addition to norepinephrine, sympathetic nerves may co-release ATP and neuropeptide Y.
- Parasympathetic Nerves: Parasympathetic nerves may co-release vasoactive intestinal polypeptide (VIP) along with acetylcholine.
- Enteric Nerves: Enteric nerves can co-release ATP, VIP, and substance P in addition to other neurotransmitters.
Functions of Autonomic Nervous System (ANS)
- The sympathetic nervous system is in charge of storing urine and feces by decreasing peristalsis and tightening sphincters.
- The parasympathetic nervous system handles the evacuation of urine and feces by increasing peristalsis and relaxing sphincters.
- Sympathetic activity typically leads to:
- Constriction of cutaneous arteries, redirecting blood to the heart, muscles, and brain.
- Increased heart rate.
- Elevated blood pressure.
- Contraction of sphincters.
- Decreased peristalsis, aiding energy mobilization for increased activity.
- Parasympathetic activity results in:
- Slower heart rate.
- Enhanced glandular and peristaltic functions in the intestines, promoting energy conservation.
- Vasoconstriction, apart from coronary arteries, is primarily driven by sympathetic signals, which also influence glands through various pathways.
- The pelvic organs, including the urinary bladder and rectum, receive support from T10–12 and L1-2 sympathetic splanchnic nerves, which:
- Decrease peristalsis in the detrusor muscle.
- Tighten the urethral sphincters to facilitate urine storage.
- The parasympathetic nervi erigentes(S2-4) stimulate:
- Increased peristalsis in the detrusor muscle.
- Relaxation of the urethral sphincters to promote urine evacuation.
- The somatic nervous systemaids in maintaining bladder and bowel control through S2-4 (somatic pudendal nerve), which:
- Tightens the external urethral sphincter (composed of skeletal muscle) to allow voluntary control over urine and feces.
- Pain signals from the bladder and upper urethra (GVA) are transmitted through:
- Pelvic splanchnic nerves.
- Inferior hypogastric plexus.
- Hypogastric nerves.
- Superior hypogastric plexus.
- Lumbar splanchnic nerves, with their cell bodies located in ganglia on the lower thoracic and upper lumbar spinal roots (T10–12; L1-2).
Parasympathetic Nervous System
- The parasympathetic nervous system is responsible for conserving energy and maintaining balance in the body. It supports calm and orderly bodily functions.
- Preganglionic cell bodies of the parasympathetic nervous system are located in specific cranial nerve nuclei in the brainstem and in the intermedio-lateral horn cells of the second to fourth sacral segments of the spinal cord.
- Efferent fibres, which are myelinated, emerge from the central nervous system (CNS) through the oculomotor, facial, glossopharyngeal, and vagus nerves, as well as in the nervi erigentes (S2-4) spinal nerves.
- Both preganglionic and postganglionic parasympathetic neurons are cholinergic, meaning they use acetylcholine as a neurotransmitter.
- The cell bodies of postganglionic parasympathetic neurons are mainly located away from the CNS, either in specific ganglia near the structures they innervate or dispersed in the walls of organs.
- In the cranial part of the parasympathetic system, there are four small peripheral ganglia: ciliary, pterygopalatine, submandibular, and otic. These ganglia are involved in efferent parasympathetic functions.
- Postganglionic parasympathetic fibres are usually unmyelinated and shorter than those in the sympathetic system. This is because the ganglia where parasympathetic fibres connect are located close to or within the organs they supply.
- The vagus nerve (CN X) provides extensive parasympathetic innervation throughout the thoracic and abdominal cavities. It contains parasympathetic preganglionic fibres with cell bodies in the medulla oblongata and visceral afferent fibres with cell bodies in the inferior (nodose) ganglion.
- Parasympathetic fibres in the vagus nerve supply all thoracic and abdominal organs, except for the descending and sigmoid colons and other pelvic organs, which are supplied by the nervi erigentes.
Sympathetic Nervous System
- The sympathetic nervous system is responsible for preparing the body for stressful or emergency situations, often referred to as the "fight or flight" response.
- It is called catabolic because it helps break down energy stores to fuel the body's response to stress.
- The sympathetic nervous system has its preganglionic cell bodies in the intermediolateral horn of the spinal cord, specifically in the segments between T1 and L2. This is why it is often referred to as thoracolumbar outflow.
- Sympathetic trunks are two ganglionated nerve cords that run alongside the vertebral column, extending from the base of the skull to the coccyx. These trunks are essential for the distribution of sympathetic fibres throughout the body.
- The sympathetic trunk primarily consists of: Ascending and descending preganglionic sympathetic fibres, Visceral afferent fibres, Cell bodies of postganglionic sympathetic fibres.
- The ganglia within the sympathetic trunk connect to spinal nerves through short connecting nerves known as white and grey rami communicantes.
- Preganglionic axons join the sympathetic trunk via the white rami communicantes, while postganglionic axons exit the trunk through the grey rami communicantes.
- In the neck region, the sympathetic trunk lies behind the carotid sheath and in front of the transverse processes of the cervical vertebrae. In the thoracic region, the trunks are located in front of the rib heads and the posterior intercostal vessels.
- The sympathetic trunks enter the abdomen through the crus of the diaphragm or behind the medial lumbocostal arch, lying anterolateral to the bodies of the lumbar vertebrae.
- In the pelvic region, the sympathetic trunks are situated in front of the sacrum and between the anterior sacral foramina. At the coccyx, the two trunks typically converge to form a single terminal ganglion.
- Cervical sympathetic ganglia often merge to form three ganglia. The internal carotid nerve, a continuation of the sympathetic trunk, arises from the superior cervical ganglion and follows the internal carotid artery into the cranial cavity.
- Generally, there are: 10 to 12 thoracic ganglia (usually 11), 4 lumbar ganglia, and 4 or 5 sacral ganglia.
- The cell bodies of preganglionic sympathetic neurons are found in the lateral horn of the spinal grey matter in all thoracic segments and the upper two or three lumbar segments. Their axons are myelinated and exit the spinal cord through the ventral nerve roots, then join the sympathetic trunk via white rami.
- Neurons similar to those in the lateral grey column can be found at other spinal levels above and below the thoracolumbar outflow, and some of their fibres may exit in other ventral roots.
Pathways of the Sympathetic Trunk
When preganglionic fibers reach the sympathetic trunk, they have several options:
- They can synapse with neurons in the nearest ganglion.
- They can ascend or descend in the sympathetic chain without synapsing, ending in another ganglion.
A preganglionic fiber has the ability to:
- Terminate in a single ganglion.
- Synapse with neurons in multiple ganglia through collateral branches.
Preganglionic fibers can also:
- Pass through the nearest ganglion, ascend or descend, and emerge in a branch of the sympathetic trunk to synapse in the ganglia of autonomic plexuses, primarily located around the celiac and mesenteric arteries.
It is possible for more than one preganglionic fiber to synapse with a single postganglionic neuron.
A unique case is the suprarenal gland, which is directly innervated by preganglionic sympathetic neurons that pass through the sympathetic trunk and celiac ganglion without synapsing.
The cell bodies of sympathetic postganglionic neurons are mainly located in:
- The ganglia of the sympathetic trunk.
- Ganglia in more peripheral plexuses.
The axons of postganglionic neurons are typically longer than those of preganglionic neurons, except for some that innervate pelvic viscera, which are shorter.
The axons of ganglionic cells are unmyelinated and reach their target organs through various pathways:
- Axons from a sympathetic trunk ganglion may return to the spinal nerve of the preganglionic origin via a gray ramus communicans. This connection occurs just before the white ramus, and the axons are then distributed through ventral and dorsal spinal rami to:
- Blood vessels (vasomotor innervation).
- Sweat glands (sudomotor innervation).
- Hair follicles (pilomotor innervation) within their specific area.
- Postganglionic fibers may travel to specific viscera via a medial branch of a ganglion, innervate nearby blood vessels, or travel externally along blood vessels to their peripheral distribution. They can also ascend or descend before leaving the sympathetic trunk.
- Many fibers are distributed along arteries and ducts as plexuses to reach distant effectors.
The sympathetic nervous system has a wider distribution compared to the parasympathetic nervous system. It innervates:
- All sweat glands.
- The arrector pili muscles.
- The muscular walls of many blood vessels.
- The heart, lungs, and respiratory tree.
- The abdominopelvic viscera.
- The esophagus.
- The muscles of the iris.
- The non-striated muscle of the urogenital tract and eyelids.
Postganglionic sympathetic fibers returning to the spinal nerves have various functions:
- They are responsible for vasoconstriction in blood vessels.
- They are secretomotor to sweat glands.
- They provide motor innervation to the arrector pili muscles within their dermatomes.
Fibers accompanying motor nerves to voluntary muscles likely only cause dilation.
Most peripheral nerves likely contain postganglionic sympathetic fibers. These fibers are involved in:
- General vasoconstriction.
- Bronchial and bronchiolar dilation.
- Modifying glandular secretion.
- Pupillary dilation.
- Inhibition of gastrointestinal muscle contraction.
Sympathetic fibers are usually associated with spinal nerves. Preganglionic sympathetic fibers may:
- Relay in their corresponding ganglion (or higher and lower ganglia) and pass to their corresponding spinal nerve for distribution.
- Pass without synapsing to a peripheral (prevertebral) ganglion for relay.
White Rami Communicantes contain preganglionic sympathetic GVE (myelinated) fibers with cell bodies located in the lateral horn (intermediolateral cell column) of the spinal cord. They also contain GVA fibers with cell bodies in the dorsal root ganglia. White rami are connected to the spinal nerves and are limited to spinal cord segments between T1 and L2.
Gray Rami Communicantes contain postganglionic sympathetic GVE (unmyelinated) fibers. These fibers supply blood vessels, sweat glands, and arrector pili muscles of hair follicles. Gray rami are connected to every spinal nerve and contain fibers with cell bodies located in the sympathetic trunk.
Thoracic Splanchnic Nerves
The Thoracic Splanchnic Nerves consist of sympathetic preganglionic GVE fibers originating from the lateral horn of the spinal cord, specifically the intermediolateral cell column. These nerves also contain GVA fibers with cell bodies located in the dorsal root ganglia. The main nerves in this group include:
- Greater Splanchnic Nerve
- Lesser Splanchnic Nerve
- Least Splanchnic Nerve
Oculosympathetic Pathway
In the oculosympathetic pathway:
- The hypothalamus (first-order neuron) transmits signals to the ciliospinal centre in the intermediolateral cell column at T1 (second-order neurons).
- The ciliospinal centre sends preganglionic sympathetic fibres to the superior cervical ganglion (third-order neuron).
- The superior cervical ganglion issues postganglionic sympathetic fibres through the tympanic cavity, cavernous sinus, and superior orbital fissure to the dilator pupillae and superior tarsal muscle (part of Muller muscle).
Disruption of this pathway can result in Horner syndrome.
Etiology
- First-order neuron injury. For instance, Wallenberg syndrome occurs due to a blockage in the posterior inferior cerebellar artery (PICA), impacting the hypothalamospinal pathway during lateral medullary ischemia.
- Second-order neuron injury. Conditions like Pancoast tumor, a form of lung cancer, can invade the sympathetic trunk. This injury may also result from cervical sympathectomy or radical neck dissection.
- Third-order neuron injury. An example of this is carotid artery dissection.
Clinical Features
- Ptosis: Partial drooping of the eyelid occurs due to paralysis of the superior tarsal muscle (a part of Muller muscle), along with the unopposed activity of the orbicularis muscle.
- Upside-down Ptosis: This condition may exhibit a slight elevation of the lower eyelid.
- Enophthalmos: This refers to a sunken globe, which can result from paralysis of the orbitalis muscle. However, it may be absent or manifest as a narrow palpebral aperture.
- Miosis: Miosis is characterized by a contracted pupil due to the paralysis of the dilator pupillae, while the sphincter pupillae remains functional. If the dilator pupillae has partial function, there may be a delay in pupillary dilation, and a light reflex might be present.
- Vasodilation: This occurs due to lesions in T-1 sympathetic vasoconstrictive fibers, leading to symptoms such as facial flushing, bloodshot conjunctiva, and nasal congestion.
- Anhydrosis: Anhydrosis refers to a lack of thermal sweating.
- Loss of the Ciliospinal Reflex: This reflex, which involves the dilation of the ipsilateral pupil in response to pain applied to the neck, face, and upper limb, is lost in Horner syndrome.
- Congenital Horner Syndrome: This condition may arise from difficult labor and hyper-abduction injury during birth, leading to the avulsion of the first thoracic nerve from the spinal cord (Klumpke’s palsy). It presents with heterochromia and unilateral straight hair.
- Heterochromia Iridis: Heterochromia iridis is characterized by a difference in color between the two eyes due to impaired melanocyte pigmentation of the iris. This impairment occurs because of a lack of sympathetic stimulation during development. As a result, the affected iris may remain blue while the other changes to brown. At birth, the iris is typically deep blue, but it may change to green or brown over time, influenced by factors such as sunlight exposure and genetics. Iris pigmentation is regulated by sympathetic factors during development, which is completed by the age of 2 years. Heterochromia is uncommon in individuals with Horner syndrome acquired later in life.
Enteric Nervous System
The enteric nervous system (ENS) is a part of the peripheral autonomic system and is made up of neurons and enteric glial cells that are organized into ganglionated plexuses. During embryonic development, some peripheral autonomic ganglia contain neurons from the neural crest that are different from the typical sympathetic and parasympathetic neurons.
The ENS is responsible for controlling various reflex functions in the gastrointestinal tract, including:
- Contractions of the muscular layers
- Secretion of gastric acid
- Intestinal movement of water and electrolytes
- Regulation of mucosal blood flow
The ENS consists of two main plexuses: the myenteric plexus (Auerbach's plexus) and the submucous plexus (Meissner's plexus), which run from the esophagus to the anal sphincter.
Although there are complex interactions between the ENS and both the sympathetic and parasympathetic systems, the ENS can maintain local reflex activity on its own, independent of the central nervous system (CNS). It continues to function even when the sympathetic and parasympathetic fibers are cut off.
In the ureter, peristalsis waves are produced by smooth muscle cells in the minor calyces, acting as a pacemaker. The sympathetic and parasympathetic nerves are not necessary for starting or spreading the contraction waves in the ureter; their role is mainly to modulate these functions.
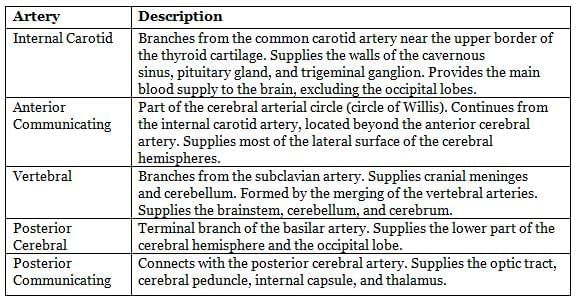
Arterial Supply
The brain receives its blood supply from two primary arterial systems: the carotid and vertebrobasilar systems. The major arteries responsible for supplying blood to the brain are detailed below.
Internal Carotid Artery
- The internal carotid artery branches from the common carotid artery and enters the carotid canal in the petrous part of the temporal bone.
- It is separated from the tympanic cavity by a thin bony structure and lies within the cavernous sinus.
- This artery gives branches to the pituitary (hypophysis) and trigeminal (semilunar) ganglion.
- The artery forms a carotid siphon, a bent tube with two arms of different lengths, just before it enters the cranial cavity.
Parts and Branches of the Internal Carotid Artery
- Cervical: No branches.
- Petrous: Caroticotympanic branch.
- Pterygoid: Cavernous branch.
- Cerebral:
- Anterior cerebral artery.
- Middle cerebral artery.
- Ophthalmic artery.
- Anterior choroidal artery.
- Posterior communicating artery.
Mnemonic for Cerebral Branches: AM-OCP
Arterial Supply to the Brain
Cerebral Arteries (AM-OCP):
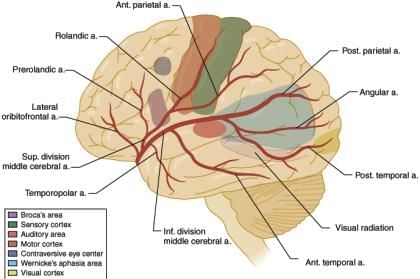
- Anterior Cerebral Artery (ACA): Enters the longitudinal fissure, supplying the optic chiasm and medial aspects of the frontal and parietal lobes. It is the primary artery for the medial cerebrum, serving the lower body representation on the brain homunculus. Blockage or hemorrhage causes sensory and motor deficits in the lower limbs and pelvic region.
- Middle Cerebral Artery (MCA): Travels laterally through the lateral cerebral fissure, supplying the lateral cerebral hemisphere. It is the main artery for the superolateral cerebrum, covering the upper body representation on the homunculus. Occlusion leads to contralateral paralysis, sensory loss in the face, neck, trunk, and arms, homonymous hemianopia, and aphasia if the dominant hemisphere is affected.
- Ophthalmic Artery: Enters the orbit via the optic canal alongside the optic nerve, supplying the eyeball, orbital structures, and forehead. Occlusion results in monocular blindness.
- Posterior Communicating Artery (PCoA): Connects the anterior and posterior circulations of the Circle of Willis, arising from the carotid siphon and joining the posterior cerebral artery. It supplies the optic chiasm, optic tract, and hypothalamus. It is the second most common site for aneurysms, which may rupture, causing subarachnoid hemorrhage and oculomotor nerve (CN III) paralysis (down-and-out eye, fixed dilated pupil, ptosis).
- Anterior Choroidal Artery: Supplies the choroid plexus of the lateral ventricles, optic tract, optic radiations, lateral geniculate body, and posterior limb of the internal capsule.
Circle of Willis:
- Located at the brain’s base in the interpeduncular fossa (subarachnoid space), it facilitates collateral blood flow during arterial occlusions.
- Composed of nine arteries: anterior communicating artery (anterior), paired anterior cerebral arteries (anterolateral), proximal segments of internal carotid arteries (lateral), paired posterior communicating arteries (posterolateral), and proximal segments of posterior cerebral arteries (posterior).
Vertebral and Basilar Arteries:
- Vertebral Artery:Originates from the subclavian artery, ascends through the foramen transversarium of C1–C6 vertebrae, curves around the atlas, pierces the dura, and enters the cranial cavity via the foramen magnum. The two vertebral arteries unite to form the basilar artery.
- Branches:
- Anterior Spinal Artery: Arises as two roots from the vertebral arteries, uniting at the foramen magnum to supply the medial medulla and anterior two-thirds of the spinal cord.
- Posterior Spinal Artery: Arises from the vertebral artery or posterior inferior cerebellar artery, supplying the posterior one-third of the spinal cord.
- Posterior Inferior Cerebellar Artery (PICA): The largest vertebral artery branch, supplies the lateral medulla and posterior-inferior cerebellum, and gives rise to the posterior spinal artery.
- Branches:
- Basilar Artery:Formed by the union of vertebral arteries at the pons’ lower border, it divides into the posterior cerebral arteries near the pons’ upper border.
- Branches:
- Pontine Arteries: Multiple branches supplying the pons.
- Labyrinthine Artery: Occasionally arises, supplying the cochlea and vestibular apparatus via the internal auditory meatus.
- Anterior Inferior Cerebellar Artery (AICA): Supplies the anterior-inferior cerebellum, providing the labyrinthine artery in 85% of cases.
- Superior Cerebellar Artery: Supplies the superior cerebellum, passing just behind the oculomotor nerve.
- Posterior Cerebral Arteries (PCAs): Supply the midbrain, thalamus, and temporal and occipital lobes, including the visual cortex. Occlusion causes contralateral sensory loss, severe pain (thalamic syndrome), and homonymous hemianopia with macular sparing.
- Branches:
Arterial Supply Overview:
- Cerebrum: Supplied by the ACA (medial), MCA (superolateral), and PCA (inferior).
- Basal Ganglia: Supplied by striate arteries (branches of ACA and MCA), thalamostriate branches of PCA, and anterior choroidal artery. Lenticulostriate artery occlusion causes contralateral hemiplegia and hemi-anesthesia due to damage to the internal capsule’s motor and sensory fibers.
- Thalamus: Supplied by posterior communicating, posterior cerebral, basilar, and sometimes anterior choroidal arteries.
- Medulla Oblongata: Supplied by vertebral, anterior and posterior spinal, PICA, and basilar arteries.
- Pons: Supplied by basilar, AICA, and superior cerebellar arteries.
- Midbrain: Supplied by PCA, superior cerebellar, and basilar arteries.
- Cerebellum: Supplied by PICA, AICA, and superior cerebellar arteries.
- Choroid Plexus: Supplied by internal carotid and PCA branches (third and lateral ventricles) and PICA (fourth ventricle).
Clinical Correlations:
Berry Aneurysms: Sac-like dilatations in the Circle of Willis, prone to rupture, causing subarachnoid hemorrhage. Common sites include:
- Anterior Communicating Artery (30–35%): Most common aneurysm site; rupture causes subarachnoid hemorrhage and bitemporal lower quadrantanopia due to optic chiasm compression.
- Posterior Communicating Artery (20–25%): Second most common site; rupture causes subarachnoid hemorrhage and oculomotor nerve palsy.
- Middle Cerebral Artery Bifurcation (20%): Occlusion leads to contralateral paralysis, sensory loss, homonymous hemianopia, and aphasia (if dominant hemisphere).
- Basilar Artery Bifurcation and Posterior Circulation: Aneurysms may compress the oculomotor nerve, causing palsy.
- Internal Carotid Artery (near termination): Aneurysms may compress the optic chiasm, causing nasal visual field defects in the ipsilateral eye.
Reflexes
Cranial Nerve Reflexes
- Corneal reflex. Afferent limb: Ophthalmic nerve
- Conjunctival reflex
- Lacrimation (tearing) reflex
- Oculocardiac reflex
- Gag reflex. Afferent limb: Glossopharyngeal nerve
- Carotid sinus reflex
- Sneezing reflex. Afferent limb: Ophthalmic/maxillary nerve
- Jaw-jerk (masseteric) reflex. Efferent limb: Mandibular nerve (Note: This is the only monosynaptic reflex mediated by the cranial nerves.)
- Papillary reflexes.
- Light reflex
- Accommodation reflex
Spinal Reflexes
Ankle jerk reflex.
- Spinal segments: S1 and S2
- Nerve: Tibial
- Muscle: Gastrocnemius
Knee jerk reflex.
- Spinal segments: L-2, 3, 4
- Nerve: Femoral
- Muscle: Quadriceps
Biceps jerk reflex.
- Spinal segments: C-5, 6
- Nerve: Musculocutaneous
- Muscle: Biceps
Supinator reflex.
- Spinal segments: C-5, 6
- Nerve: Radial
- Muscle: Brachioradialis
Triceps reflex.
- Spinal segments: C-7, 8
- Nerve: Radial
- Muscle: Triceps
Memory Aid: S-1; L-2, 3, 4; C-5, 6; C-7, 8.
|
68 docs|16 tests
|
FAQs on Neuroanatomy - 4 Chapter Notes - Anatomy - NEET PG
| 1. What is the function of the Spinothalamic Tract (STT) in the nervous system? |  |
| 2. How does the Pyramidal System differ from the Extrapyramidal System? |  |
| 3. What are the primary functions of the Autonomic Nervous System, and how is it divided? |  |
| 4. What role do the Thoracic Splanchnic Nerves play in the sympathetic nervous system? |  |
| 5. Can you explain the concept of reflex arcs and their importance in the nervous system? |  |















