Thorax - 1 Chapter Notes | Anatomy - NEET PG PDF Download
Surface Markings and Anatomical Landmarks
The horizontal sternal plane is commonly considered to pass through the intervertebral disc situated between the fourth and fifth thoracic vertebrae in the posterior aspect of the thoracic cavity.
Sternal Angle (of Louis)
- The sternal angle, also known as the angle of Louis, is found at the junction where the manubrium meets the body of the sternum.
- This landmark signifies several important anatomical levels, including:
- The point where the second rib (specifically its costal cartilage) attaches to the sternum.
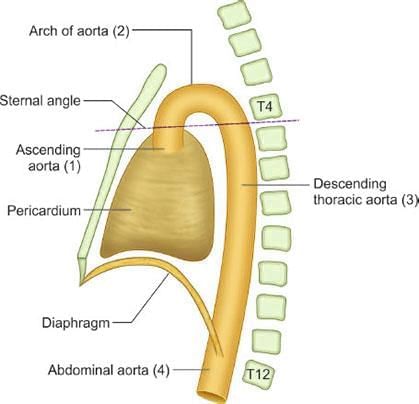
- The aortic arch, which begins and ends at the level of the T4 vertebra.
- The bifurcation of the trachea into the right and left primary bronchi.
- The division of the pulmonary trunk into the right and left pulmonary arteries.
- The upper boundary of the heart.
- The entry point of the superior vena cava into the right atrium, passing through the pericardium.
- The demarcation between the superior and inferior mediastinum.
- The arching of the azygos vein over the root of the right lung to join the superior vena cava.
The arch of the aorta is located at the same level as the sternal angle, corresponding to the T4 vertebra.
Development of Cardiovascular System
- Origin of Heart Tissues: The heart develops from the midline splanchnopleuric coelomic epithelium, with contributions from neural crest mesenchyme.
- Formation of Myocardium: The splanchnopleuric coelomic epithelium forms the myocardium, including the heart's conduction system.
- Endocardium and Valve Tissues: The endocardium and cardiac mesenchymal cells produce the heart's valve tissues.
- Epicardium and Coronary Arteries: The splanchnopleuric coelomic epithelium also produces the epicardium, coronary arteries, and interstitial fibroblasts.
- Migration of Heart Progenitor Cells: Around day 16, heart progenitor cells migrate through the primitive streak to form the primary heart-forming regions in the splanchnic layer of lateral plate mesoderm.
- Cardiogenic Area: This area is located at the embryo's head end, between the septum transversum and prochordal plate.
- Formation of Heart Tube: The heart tube develops from the mesoderm surrounding the endocardium.
- Cardiac Jelly: Myocardial cells secrete cardiac jelly, an extracellular matrix rich in hyaluronic acid, which accumulates between the endothelium and myocardium.
- Endocardial Cushions: Cardiac jelly accumulates within the endocardial cushions, which are precursors of cardiac valves.
- Epicardium Formation: Mesoderm migrating from the coelomic wall near the liver forms the epicardium.
- Detection of Heart beat: The heartbeat becomes detectable around day 22 of intrauterine life.
- Blood Flow Observation: Blood flow during the fourth week can be observed using Doppler ultrasonography.
- Dilatations of Heart Tube: The heart tube develops five dilatations: sinus venosus, primitive atrium, primitive ventricle, bulbus cordis, and truncus arteriosus.
- Adult Derivatives of Dilatations:
- Truncus arteriosus: Ascending aorta
- Bulbus cordis: Smooth upper part of the right ventricle (Conus arteriosus) and smooth upper part of the left ventricle (aortic vestibule)
- Primitive ventricle: Trabeculated part of the right ventricle and trabeculated part of the left ventricle
- Primitive atrium: Trabeculated part of the right atrium and trabeculated part of the left atrium
- Sinus venosus: Smooth part of the right atrium (sinus venarum), coronary sinus, and oblique vein of the left atrium
- Division of Truncus Arteriosus: The truncus arteriosus divides into the ascending aorta and pulmonary trunk by forming the aorticopulmonary (AP) septum.
- Dextral Looping: During the fourth week, the dilations undergo dextral looping, completed by day 28.
- Positioning of Atria and Ventricles: The atria move to a posterior position, while the ventricles shift forward to a more anterior location.
- Support of Heart Tube:. dorsal mesocardium initially supports the heart tube, later developing into the transverse pericardial sinus.
- Right Horn of Sinus Venosus: The right horn of the sinus venosus merges into the back part of the primitive atrium, forming the sinus venarum.
- Sulcus Terminalis: The sulcus terminalis marks the boundary between the smooth and rough areas of the right atrium, indicated internally by the crista terminalis.
- Crista Terminalis: The crista terminalis is a vertical muscular ridge serving as the origin for the pectinate muscles.
- Left Horn of Sinus Venosus: The left horn of the sinus venosus develops into the coronary sinus, which opens into the back wall of the right atrium.
- Formation of Superior and Inferior Vena Cava: The superior vena cava and inferior vena cava form from the cardinal veins and open into the right atrium.
- Formation of Pulmonary Veins: Pulmonary veins arise in the dorsal mesocardium and connect to the back wall of the left atrium.
- Coronary Arteries and Veins: Coronary arteries and veins are regarded as the vasa-vasorum of the heart.
The entrance of the sinus venosus into the primitive atrium is protected by the left and right venous valves.
- Left Venous Valve: Fuses with the interatrial septum along with the septum spurium.
- Right Venous Valve: Stretches and splits into three parts due to superior and inferior limbic bands, forming:
- Crista terminalis (upper part).
- Eustachian valve (valve of inferior vena cava, middle part).
- Thebesian valve (valve of coronary sinus, lower part).
- Eustachian Valve: A rudimentary semilunar valve at the inferior vena cava opening, derived partly from the right venous valve and partly from the sinus septum.
- Thebesian Valve: An incomplete semicircular valve at the coronary sinus opening, formed from the lower right venous valve.
- Heart Tube Formation: Occurs on day 22 (week 4) within hyaluronic acid secreted by the myocardium.
- Heart Development Completion: Fully developed by the 10th week (3rd month) of intrauterine life.
- Coronary Sinus Formation: The left horn of the sinus venosus regresses to form the coronary sinus.
Septa Formation
The heart is divided into four chambers by the formation of the septum and valves.
Four Main Septa:
- AV Septum
- Atrial Septum
- Interventricular Septum
- AP Septum
Development of Septum
The septum in the heart develops from the growth of endocardial cushion tissue in the atrioventricular canal and the cono-truncal area.
AV Septum
Endocardial Cushions:
- Four endocardial cushions surround the atrioventricular canal.
- The dorsal and ventral AV endocardial cushions join to form the AV septum, splitting the orifice into the right and left atrioventricular canals.
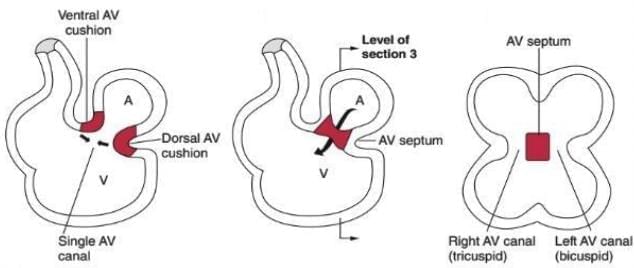
Transformation to Fibrous Tissue:
- The cushion tissue eventually changes into fibrous tissue.
- This forms the mitral (bicuspid) valve on the left and the tricuspid valve on the right.
Development of the Atria and Interatrial Septum
The formation of the atria involves both the growth of the original atrial area and the incorporation of new structures.
Right Atrium
- The sinus venosus is integrated into the right atrium, creating the smooth part known as the sinus venarum. This area is separated from the trabeculated section by the crista terminalis.
- The crista terminalis itself is formed from the ridge of the inferior vena cava (IVC) and the valve of the coronary sinus.
- The rough trabeculated part of the right atrium, located in front of the crista terminalis, and the right auricle, develop from the primitive atrium (right half), the right venous valve, and the right half of the atrioventricular (AV) canal.
Left Atrium
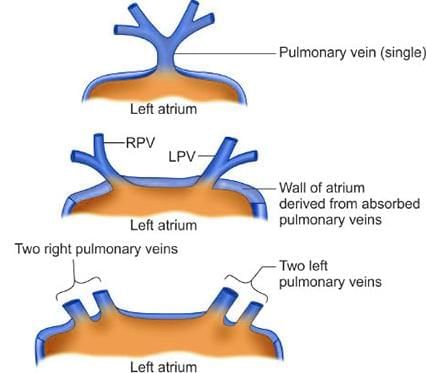
- The left atrium's posterior smooth part, located between the openings of the pulmonary veins, develops from the absorption of the pulmonary veins into the atrium.
- The anterior rough part of the left atrium and the left auricle originate from the left half of the primitive atrium and the left half of the AV canal.
Interatrial Septum
- The septum primum grows towards the floor of the atrium, and as it extends, it carries with it cells from the dorsal mesenchyme.
- Eventually, the base of the pulmonary vein merges into the left atrium as the atrium expands, leading to the formation of the smooth area of the left atrium.
- This process continues until the four branches of the pulmonary vein enter the atrium, establishing the smooth posterior wall of the left atrium.
Components of the Right and Left Atria in Adults and Their Embryonic Sources
Right Atrium:
- Rough trabeculated part (atrium proper) in front of the crista terminalis
- Right auricle
- Smooth part behind the crista terminalis (sinus venarum)
Left Atrium:
- Posterior smooth part between the openings of the pulmonary veins
- Anterior rough part and left auricle
- Absorption of pulmonary veins near the atria
Development of Interatrial Septum
- In fetal circulation, oxygenated blood from the placenta flows into the right atrium and directly into the left atrium, bypassing the inactive lungs.
- The primitive atrium is initially divided by the septum primum, which grows downwards from the top of the atrium towards the atrioventricular cushions.
- The septum primum, shaped like a sickle, starts to split the atrium into two sides while maintaining a passage called the ostium primum for blood flow between them.
- The ostium primum is eventually closed when the septum primum fuses with the endocardial cushions, creating the ostium secundum through cell death in the septum primum.
- A second membrane, the septum secundum, grows down from the lower front wall towards the cushions but does not connect with them. It covers most of the ostium secundum, forming a flap known as the foramen ovale, which allows blood to flow from the right atrium to the left.
- At birth, when the pressure in the left atrium increases, the two septa press together, closing the connection between the two atria, a process usually finalised around three months after birth.
- As the septum primum and septum secundum join together, the foramen ovale in the septum secundum is pressed closed by the septum primum.
- The fossa ovalis is a depression on the interatrial septum with a thin fibrous tissue sheet at the bottom, a remnant of the septum primum.
- The limbus fossa ovalis is the prominent horseshoe-shaped edge of the fossa ovalis, marking the border of the fetal septum secundum.
Development of Pulmonary Veins
- The pulmonary vein originates in the dorsal mesocardium.
- As the left atrium expands, the pulmonary vein becomes part of it, with the four branches of the vein entering the atrium's back wall.
- Some cardiologists propose that the pulmonary vein comes from an outgrowth of the dorsal atrial wall.
- This concept relates to stages of embryonic heart development, as observed in recent cardiology research.
AP Septum and Anomalies
Partition of Truncus Arteriosus and Bulbus Cordis
- Formation of AP Septum: Truncal and bulbar ridges, originating from neural crest mesenchyme, grow spirally and merge to form the aorticopulmonary (AP) septum.
- Division of Truncus Arteriosus: The spiral AP septum divides the truncus arteriosus into the proximal aorta and pulmonary artery, with the resulting vessels spiraling around each other.
- Division of Bulbus Cordis: The bulbus cordis splits into the smooth-walled part of the right ventricle, the conus, and the truncus arteriosus.
- Cono-Truncal Anomalies: Abnormal division of the cono-truncal region can lead to AP septum anomalies such as Persistent Truncus Arteriosus (PTA), Transposition of Great Vessels (TGV), and Tetralogy of Fallot (TOF), causing right-to-left shunting, inadequate blood oxygenation, and cyanosis.
Persistent Truncus Arteriosus (PTA)
- Cause: Failure of cono-truncal ridges to fuse and descend toward the ventricles results in the absence of the AP septum, leading to PTA.
- Outcome: No ascending aorta or pulmonary trunk forms; a single primitive truncus arteriosus persists, causing blood mixing and cyanosis.
Transposition of Great Vessels (TGV)
Cause: A non-spiral AP septum results in non-spiraled great vessels that connect to the wrong ventricles, leading to transposition.
Outcome: The aorta originates from the right ventricle, and the pulmonary artery arises leftward and posteriorly from the left ventricle, creating two separate parallel circulations. This causes right-to-left shunting and cyanosis. Post-birth survival requires communication between circulations, often via an interatrial communication, a patent ductus arteriosus (in two-thirds of cases), or a ventricular septal defect (VSD, in one-third of cases).
Tetralogy of Fallot (TOF)
Cause: Misalignment of the AP septum (anterior migration) with the atrioventricular (AV) septum results in four defects: (1) pulmonary stenosis (right ventricular outflow obstruction), (2) VSD, (3) overriding aorta (aorta positioned over both ventricles due to the VSD), and (4) right ventricular hypertrophy.
Outcome: Right-to-left shunting and cyanosis occur due to these structural abnormalities.
Overriding Aorta Definition: The aorta's outlet is positioned over both ventricles (instead of solely the left ventricle), directly above the VSD, causing the aorta to arise from both ventricles.
Fetal Circulation
The blood that is rich in oxygen and nutrients travels from the placenta to the fetus through a vessel called the left umbilical vein.
- Most of this blood bypasses the liver sinusoids by passing through a channel known as the ductus venosus into the inferior vena cava (IVC).
- From the IVC, the blood enters the right atrium of the heart. Here, most of the blood skips the right ventricle (and, consequently, the lungs) by flowing through the foramen ovale into the left atrium.
- Blood then moves from the left atrium to the left ventricle and is pumped to the fetal tissues via the aorta.
- Deoxygenated fetal blood returns to the placenta through the right and left umbilical arteries, which branch off from the internal iliac arteries.
- Some blood in the right atrium goes to the right ventricle, and blood from the right ventricle enters the pulmonary trunk, but most of it bypasses the lungs through the ductus arteriosus.
 Changes at Birth
Changes at Birth
- At birth, when the baby takes its first breath, the pressure in the left atrium increases. This rise in pressure causes the foramen ovale to close, as the septum primum pushes against the septum secundum.
- Initially, there is an increase in blood flow through the pulmonary artery, but the blood is poorly oxygenated because it is receiving systemic venous blood.
- As the baby continues to breathe, pulmonary vascular resistance decreases, leading to an increase in blood flow to the lungs.
- The ductus arteriosus gradually closes over the next few hours to days after birth.
- The changes that occur include the closure of the right and left umbilical arteries, the left umbilical vein, the ductus venosus, the ductus arteriosus, and the foramen ovale.
- When the placenta is removed, tying off the umbilical cord leads to thrombosis of the umbilical arteries, which transform into the medial umbilical ligaments. The umbilical vein becomes the ligamentum teres, and the ductus venosus transforms into the ligamentum venosum.
- These embryological remnants create corresponding peritoneal folds on the anterior abdominal wall.
Peritoneal Folds on the Anterior Abdominal Wall
- The falciform ligament houses the ligamentum teres, which is the remnant of the left umbilical vein in adults, directing towards the liver.
- The medial umbilical fold is formed by the medial umbilical ligament, the adult remnant of the distal umbilical arteries.
- The median umbilical fold is created by the urachus, the adult remnant of the allantois.
- The lateral umbilical fold is elevated by the inferior epigastric vessels.
- Note: In adults, the proximal part of the umbilical artery is present as superior vesical arteries.
- The physiological closure of the ductus arteriosus occurs within 1–4 days after birth.
- In a typical full-term infant, a small amount of blood flow usually continues for 24 to 48 hours.
- After 24 hours (one day), 20% of ducts are functionally closed; 82% by 48 hours. and 100% at 96 hours (4 days).
- The anatomical closure of the ductus arteriosus takes place within 2–12 postnatal weeks (1 month to 3 months).
- The ductus arteriosus closes by 8 weeks in 88% of children with a normal cardiovascular system.
- Anatomical closure involves proliferation and fibrosis of the tunica intima.
Ribs
Development
- The process of endochondral ossification in ribs begins near the angle of the rib, around the end of the second month of fetal development, with initial appearances in the sixth and seventh ribs.
- Ribs usually develop in conjunction with the thoracic vertebrae.
- Each rib originates from lateral sclerotome populations, which are formed from the caudal half of one sclerotome and the cranial half of the sclerotome below it.
Articulation
- The head of a rib articulates with the corresponding vertebral body, the intervertebral disc, and the upper vertebral body.
Types of Ribs
- The human ribcage consists of various types of ribs:
- Typical Ribs: Ribs 3 to 9, which share similar characteristics.
- Atypical Ribs: Ribs 1, 2, 10, 11, and 12, each with unique features.
- True Ribs. Ribs 1 to 7, also known as the upper 7 ribs.
- False Ribs. Ribs 8 to 12, known as the lower 5 ribs.
- True ribs are connected to the sternum at the front. In contrast, false ribs are attached to the costal cartilages of the true ribs positioned above them, contributing to the formation of the front costal margin.
- Vertebro-sternal Ribs. Ribs 1 to 7, which connect to the vertebrae at the back and to the sternum at the front.
- Vertebro-chondral Ribs. Ribs 8 to 10, connecting to the vertebrae at the back, with their cartilages meeting the cartilage of the upper rib at the front.
- Vertebral (Floating) Ribs. Ribs 11 and 12, which connect to the vertebrae but do not attach to the sternum.
- The first seven true ribs connect to the sternum through costal cartilages.
- The five false ribs are connected either to their respective costal cartilage (ribs 8 to 10) or have free-floating front ends (ribs 11 and 12).
Joints
- Sternochondral (also called Sternocostal. joints link the sternum to the first seven cartilages.
- The costal cartilage of the first rib attaches to the manubrium sternii via a fibrocartilage plate, making it an atypical primary cartilaginous (symphysis) joint, allowing no movement.
- Costal cartilages from the second to the seventh ribs form plane synovial joints with the sternum, permitting free movement.
- The first rib's connection to the sternum (first sterno-costal joint) is a distinct type of synarthrosis, often mistakenly classified as a primary cartilaginous (symphysis) joint.
- Ribs two to seven attach to the sternum through synovial joints.
- Ribs six to nine interconnect via synovial joints (Interchondral joints), with some fibrous connections.
- The eighth, ninth, and tenth ribs connect to the seventh rib using costal cartilage.
- The manubriosternal joint is a symphysis (secondary cartilaginous) joint.
- The xiphisternal joint is a primary cartilaginous (symphysis) joint, although some references classify it as a symphysis.
- Note: The joints between the rib's front end and costal cartilage (costo-chondral joint) are primary cartilaginous (symphysis) joints, allowing no movement.
- The first rib is the broadest and shortest of the true ribs, featuring two grooves for the subclavian artery and vein.
- SVAN structures are situated between the first rib and the lung's apex (from medial to lateral): S - Sympathetic trunk, V - Vein (intercostal), A - Artery (superior intercostal), N - Nerve (T1 nerve).
- The inner border (scalene tubercle) is where the scalenus anterior muscle attaches, and it is also linked to Sibson’s (suprapleural membrane) fascia.
- The second rib has two articular facets on its head, connecting with the bodies of the second and first thoracic vertebrae. It is about twice as long as the first rib.
- The first rib is the widest and most curved, while the twelfth rib is the narrowest and smallest.
- The seventh rib is the longest, the eighth rib projects the most laterally, and the ninth rib is the most oblique.
- The tenth rib has a single articular facet on its head, which connects with the tenth thoracic vertebra.
- The eleventh and twelfth ribs each have a single articular facet on their heads, and they lack a neck or tubercle.
Nervous Supply of Thorax
Thoracic Spinal Nerves
- The intercostal nerves are formed by twelve pairs of thoracic spinal nerves.
- These nerves are responsible for supplying the muscles and skin in the intercostal spaces, with the lower nerves also serving the anterolateral abdominal wall.
- Specifically, the intercostal nerves are the anterior (ventral) branches of the first 11 thoracic spinal nerves.
- The 12th nerve, known as the subcostal nerve, arises from the ventral ramus of T12.
- These nerves run between the internal and innermost muscle layers, accompanied by the intercostal veins and arteries.
- They are located in the costal grooves on the underside of the ribs, providing both muscular and cutaneous branches.
- Typical intercostal nerves include the 3rd, 4th, 5th, and 6th, which remain within their respective intercostal spaces.
- Atypical intercostal nerves include the 1st, 2nd, 7th, 8th, 9th, 10th, and 11th, extending beyond the thoracic wall to supply other areas.
- The T1-T2 nerves also supply the upper limb through the brachial plexus (T1) and the intercostobrachial nerve (T2).
- The T7-T11 nerves provide innervation to the abdominal wall.
- The T12 nerve supplies the abdominal wall and the skin of the buttock.
- The intercostobrachial nerve, a branch of the 2nd intercostal nerve, innervates the skin in the axilla and the upper inner arm.
- This nerve can be involved in referred cardiac pain and may be injured during axillary node clearance (ANC) in breast cancer surgery.
- The subcostal nerve (T-12) originates from the ventral ramus of T12, following the bottom edge of the 12th rib into the abdominal wall, where it supplies the abdominal wall and skin in the gluteal region.
- The phrenic nerve arises from the anterior primary rami of C3-C5 (primarily C4) and carries motor, sensory, and sympathetic fibers.
- It descends along the front of the scalene anterior muscle, covered by the sternocleidomastoid muscle at the root of the neck, then enters the thorax, accompanying the pericardiophrenic artery.
- Within the thorax, the phrenic nerve passes in front of the lung's root (hilum), lying between the mediastinal pleura and the fibrous pericardium, supplying both structures.
- The right phrenic nerve is shorter and more vertical, while the left phrenic nerve is longer and follows a more oblique path.
- The right dome of the diaphragm is higher due to the presence of the liver, whereas the left dome is lower because of the heart.
- The phrenic nerve is the sole motor supply to the diaphragm and carries sensory information from the central diaphragm, peritoneum, pleura, and pericardium along its course.
- Pain from pericarditis is transmitted by the phrenic nerve and originates from the parietal layer only.
- The fibrous and parietal layers of the serous pericardium are supplied by the phrenic nerve, while the visceral layer is insensitive to stretch.
Arterial Supply in the Thorax
- The Internal Thoracic Artery originates from the first part of the subclavian artery. It runs downward, situated behind the first six costal cartilages and close to the sternum.
- This artery gives rise to two anterior intercostal arteries in each of the upper six intercostal spaces. It terminates at the sixth intercostal space, where it bifurcates into the musculophrenic artery and the superior epigastric artery.
The pericardiophrenic artery, a branch of the internal thoracic artery, accompanies the phrenic nerve between the pleura and the pericardium to the diaphragm. It supplies blood to the pleura, pericardium, and the upper part of the diaphragm.
- The anterior intercostal arteries for intercostal spaces 1 to 6 are derived from the internal thoracic artery. In contrast, those for spaces 7 to 9 are supplied by the musculophrenic artery.
- Each intercostal space contains two anterior intercostal arteries: one at the upper border and one at the lower border.
- The upper artery in each intercostal space connects with the posterior intercostal artery, while the lower artery connects to the collateral branch of the posterior intercostal artery.
- These arteries also provide muscular branches to the intercostal, serratus anterior, and pectoral muscles.
- The anterior perforating branches, specifically the second, third, and fourth, supply medial mammary branches to the breast.
The musculophrenic artery runs along the costal arch, on the inner side of the costal cartilages. It gives rise to two anterior intercostal arteries in the 7th to 9th intercostal spaces. After passing through the diaphragm, it terminates in the 10th intercostal space, where it connects with the deep circumflex iliac artery.
- This artery supplies blood to the pericardium, diaphragm, and abdominal wall muscles.
The superior epigastric artery descends on the deep surface of the rectus abdominis muscle within the rectus sheath. It supplies this muscle and forms anastomoses with the inferior epigastric artery within the rectus sheath.
- This artery provides blood to the diaphragm, peritoneum, and anterior abdominal wall.
The posterior intercostal arteries for intercostal spaces 1 and 2 are branches of the superior intercostal artery, which itself is a branch of the costocervical trunk of the subclavian artery. The arteries for spaces 3 to 11 arise from the descending thoracic aorta.
- In each intercostal space, the posterior intercostal arteries are located between the internal and innermost intercostal muscles, positioned between the intercostal vein (above) and the intercostal nerve (below).
- They supply blood to the intercostal muscles, overlying skin, and parietal pleura.
- Notably, the right posterior intercostal arteries are longer than their left counterparts.
Mammary branches are derived from the posterior intercostal arteries of the 2nd, 3rd, and 4th intercostal spaces. These branches supply blood to the mammary gland.
The right bronchial artery typically arises from the right main bronchus or the right intercostal arteries, rather than specifically from the 3rd posterior intercostal artery.
The superior (highest) intercostal artery is a branch of the costocervical trunk. It descends in front of the neck of the first two ribs, giving rise to posterior intercostal arteries for the first two intercostal spaces.
Aorta
The ascending aorta starts from the left ventricle within the pericardial sac and rises behind the sternum, ending at approximately the sternal angle.
Positioned in the middle mediastinum, it features three aortic sinuses above the aortic valve cusps and branches into the right and left coronary arteries.
The arch of the aorta, extending from the ascending aorta, begins and ends slightly to the right at the upper edge of the right second sternocostal joint. It ascends, bends backward and left, passing in front of the trachea's bifurcation, then curves down behind the left bronchus, descending to the left of the fourth thoracic vertebra as the descending thoracic aorta.
The arch terminates at the sternal end of the left second costal cartilage, remaining entirely within the superior mediastinum (behind the lower half of the manubrium sterni).
The arch of the aorta gives rise to three major branches:
- Brachiocephalic artery
- Left common carotid artery
- Left subclavian artery
The descending thoracic aorta begins at the fourth thoracic vertebra, descending alongside the vertebral column on the left side before passing through the aortic hiatus of the diaphragm at the T12 vertebral level. It gives rise to nine pairs of posterior intercostal arteries and one pair of subcostal arteries, along with branches for the pericardium, bronchial (one right and two left), esophageal, mediastinal, and superior phrenic regions.
Coarctation of the aorta refers to the narrowing of the aorta due to a defect in the tunica media, resulting in a shelf-like projection into the lumen, commonly near the ductus arteriosus. There are three types of coarctation:
- Pre-ductal coarctation. narrowing occurs before the ductus arteriosus. Severe cases require a patent ductus arteriosus for blood flow to the aorta below the narrowing, making closure potentially life-threatening.
- Ductal coarctation. narrowing occurs at the ductus arteriosus insertion, typically appearing when the ductus arteriosus closes.
- Post-ductal coarctation. narrowing occurs after the ductus arteriosus insertion. Even with an open ductus arteriosus, blood flow to the lower body can be compromised.
The postductal type of coarctation may allow for years of normal life by facilitating the development of extensive collateral circulation to the aorta below the stenosis.
- The arch of the aorta gives rise to the subclavian artery, which branches into the internal thoracic artery, leading to the anterior intercostal artery. This connects to the posterior intercostal artery, which feeds into the descending thoracic aorta, supplying the thorax, abdomen, pelvis, and lower limbs.
- From the arch of the aorta, the subclavian artery branches into the costocervical trunk, which forms the superior intercostal artery. This leads to the third posterior intercostal artery, connecting to the descending thoracic aorta, supplying the thorax, abdomen, pelvis, and lower limbs.
- The scapular anastomosis involves the dorsal scapular artery, which connects to the posterior intercostal artery, leading to the descending thoracic aorta, supplying the thorax, abdomen, pelvis, and lower limbs.
- The arch of the aorta branches into the subclavian artery, which gives rise to the internal thoracic artery. This forms the superior epigastric artery, which connects to the inferior epigastric artery and iliac artery, supplying the pelvis and lower limbs.
|
42 docs|7 tests
|
FAQs on Thorax - 1 Chapter Notes - Anatomy - NEET PG
| 1. What is the process of development of the interatrial septum and its significance in the heart's anatomy? |  |
| 2. How are the pulmonary veins formed during embryonic development? |  |
| 3. What is the partitioning of the truncus arteriosus and bulbus cordis, and why is it important? |  |
| 4. What are the characteristics and implications of persistent truncus arteriosus (PTA)? |  |
| 5. What are the defining features of transposition of great vessels (TGV) and its impact on circulation? |  |















