Anticoagulants: Coagulation Process | Zoology Optional Notes for UPSC PDF Download
| Table of contents |

|
| Coagulation Process: Platelets and Clotting Factors |

|
| Anticoagulants |

|
| Antiplatelet Drugs |

|
| Special Considerations in Anticoagulant Therapy |

|
| Comparison of Anticoagulant Therapies |

|
Coagulation Process: Platelets and Clotting Factors
- Initiation of Coagulation: Platelets and clotting factors play crucial roles in initiating the coagulation process. When an injury occurs, platelets (thrombocytes) rapidly move toward the damaged area. Their functions include aggregation, where platelets stick together, and adhesion, where they adhere to the vessel walls. This dual action forms a plug around the injured tissue.
- Platelet Plug Formation: The immediate response to injury involves platelets forming a plug around the damaged tissue. This process is vital for minimizing blood loss and preventing further damage. Platelet aggregation ensures the rapid formation of a protective barrier.
- Interaction with Plasma Clotting Factors: Simultaneously, plasma clotting factors, present in the blood, reach the platelet plug. These clotting factors interact with each other in a cascade-like manner, leading to the formation of a stable blood clot. This clotting process is highly regulated and involves various factors working in concert to achieve hemostasis.
- Hemostasis: Hemostasis refers to the delicate balance between clot formation and clot breakdown, and it is a continuous process that occurs throughout the day. The goal is to prevent excessive bleeding while maintaining blood fluidity. The coagulation system operates under tight control to ensure that blood clots form only when necessary, and they are appropriately dissolved after the injury is healed.
In summary, the coagulation process involves the rapid response of platelets to the site of injury, their aggregation and adhesion to form a plug, and the subsequent interaction with plasma clotting factors to create a stable blood clot. Hemostasis, the equilibrium between clot formation and dissolution, is crucial for maintaining vascular integrity and preventing excessive bleeding.
Anticoagulants
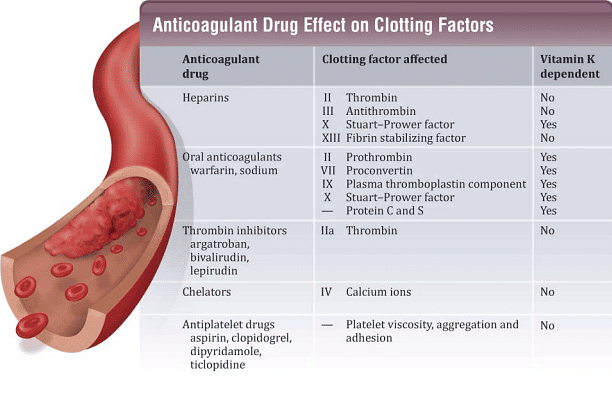
Clinically useful anticoagulants exert their pharmacological effects by interfering with plasma clotting factors, inhibiting platelet aggregation, or dissolving clots. The mechanism of anticoagulation is crucial in determining the onset and duration of drug action.
- Heparin: Quick Onset and Duration: Heparin acts quickly, and its anticoagulant effect is immediate upon the formation of the thromboplastin-drug complex.
- Warfarin: Long Onset and Duration: Warfarin, on the other hand, has a delayed onset and a prolonged duration of action. It takes days to clear the normal clotting factors before the anticoagulant effect becomes evident.
- Antiplatelets: Antiplatelet drugs function by inhibiting platelet aggregation, preventing the formation of the platelet plug, or blocking platelet adhesion to the vessel walls. These drugs reduce platelet stickiness by directly inhibiting adenosine diphosphate (ADP)-mediated platelet aggregation.
- Thrombolytics: Thrombolytics operate by either forming complexes with plasminogen activator proteins (e.g., streptokinase) or directly with the activator protein tissue plasminogen activator (tPA). These drugs interfere with stage four of clot formation.
In summary, anticoagulants interfere with clotting factors, antiplatelets inhibit platelet aggregation, and thrombolytics disrupt the formation of blood clots by interacting with plasminogen activators or tPA. The choice of medication depends on the specific clinical scenario and the desired therapeutic outcome.
Antiplatelet Drugs
Antiplatelet drugs play a crucial role in inhibiting platelet aggregation, preventing the formation of the platelet plug, and blocking platelet adhesion to vessel walls. Here are some commonly used antiplatelet drugs:
Aspirin:
- Mechanism: Alters cyclooxygenase needed to generate thromboxane, a potent platelet aggregator and vasoconstrictor.
- Irreversible: Aspirin's effects are irreversible, requiring the formation of new platelets for recovery (which can take a few hours).
Clopidogrel (Plavix) and Ticlopidine (Ticlid):
- Mechanism: Block adenosine diphosphate (ADP) receptors on platelet cell membranes, preventing the activation of glycoproteins IIa/IIIB. These glycoproteins are essential for the crosslinking of platelets to fibrin.
- Effect: Inhibits platelet aggregation.
Dipyridamole (Persantine):
- Mechanism:
- Increases extracellular adenosine (an inhibitor of platelet reactivity) by decreasing the reuptake of adenosine in platelets, red blood cells (RBCs), and endothelial cells.
- Inhibits phosphodiesterase enzyme, increasing cyclic adenosine monophosphate (cAMP) in the cell and blocking the platelet response to ADP.
- Mechanism:
Side Effects of Antiplatelet Drugs:
- Headache
- Vomiting
- Rash
- Dizziness
- Diarrhea
Specific Side Effects of Ticlopidine and Clopidogrel:
- Thrombocytopenia (reduced platelet count)
Antiplatelet drugs are crucial in preventing pathological blood clot formation, especially in conditions like cardiovascular diseases. The choice of drug depends on the patient's condition, and side effects need to be carefully monitored.
Special Considerations in Anticoagulant Therapy
- Anticoagulant therapy should be administered consistently at the same time each day.
- Patients should be closely observed for signs of increased bleeding or hemorrhage.
- Careful examination of heparin vials is essential to determine the correct strength.
- Patients with active bleeding should not receive anticoagulants.
Monitoring Coagulation:
- Therapeutic dosage is evaluated based on clotting time, including tests like Partial Thromboplastin Time (PTT), Prothrombin Time (PT), International Normalized Ratio (INR), and Activated Partial Thromboplastin Time (APTT).
- Drugs affecting platelet aggregation can lead to increased bleeding.
- Warfarin has a higher potential for drug interactions.
Fibrinolytic/Thrombolytic Drugs:
- Clot busters: Dissolve preformed blood clots.
- Examples include Urokinase, Streptokinase, Alteplase, Tenecteplase, and Reteplase.
- Used to lyse pulmonary and coronary artery thrombosis.
- Major adverse effect is hemorrhage.
Comparison of Anticoagulant Therapies
Preferred Therapy:
- Heparin:
- Indicated for venous thrombosis and pulmonary embolism.
- Warfarin:
- Used for prophylaxis of venous thrombosis and pulmonary emboli.
- Antiplatelets:
- Employed in coronary artery disease.
- Thrombolytics:
- Utilized for the dissolution of preformed clots.
Each type of anticoagulant therapy has its specific indications and preferred uses, tailored to the patient's condition and the desired therapeutic outcome. Monitoring and careful management are crucial to ensuring the efficacy and safety of these treatments.
|
181 videos|351 docs
|















