Nonalcoholic Fatty Liver Diseases and Nonalcoholic Steatohepatitis (NAFLD/NASH) | Medical Science Optional Notes for UPSC PDF Download
Epidemiology
- Non-Alcoholic Fatty Liver Disease (NAFLD) is the most prevalent liver disease in Western countries and is rapidly increasing as a form of chronic liver disease globally.
- It is projected to become the primary reason for liver transplantation in the United States by 2020.
- The escalating rates of childhood obesity indicate that NAFLD will likely contribute even more significantly to the overall burden of liver disease in the future.
- NAFLD is considered a premalignant condition.
- It is strongly linked to overweight/obesity and insulin resistance.
- The documented prevalence of NAFLD varies, being lowest in African Americans (approximately 25%), highest in Americans of Hispanic ancestry (around 50%), and intermediate in American whites (about 33%).
- Heritable factors play a role.
- Variants in the PNPLA3 gene, involved in intracellular lipid trafficking, consistently correlate with susceptibility to hepatic steatosis, cirrhosis, and liver cancer.
- Polymorphisms in genes TM6SF2 and MBOAT7 are also emerging as potential genetic risk factors for NAFLD.
Pathogenesis
- NAFLD Progression Spectrum:
- Begins with Hepatic Steatosis, advances to Steatohepatitis (NASH), and can lead to Cirrhosis and Liver Cancer.
- Mechanisms of NAFLD Pathogenesis and Progression:
- The mechanisms behind NAFLD development and progression are not fully understood.
- Hepatocyte mechanisms involved in triglyceride synthesis overpower mechanisms for triglyceride disposal, resulting in intracellular fat accumulation.
- This leads to increased hepatocyte death, with dying hepatocytes releasing factors that trigger wound healing responses, attempting to regenerate lost hepatocytes, ultimately resulting in NASH.
- Cirrhosis develops due to inefficient repair, marked by the progressive accumulation of wound healing cells, fibrous matrix, and abnormal vascular structures, rather than efficient reconstruction/regeneration of the hepatic parenchyma.
- Primary liver cancers occur when malignantly transformed liver cells escape normal control over regenerative growth.
- Prevalence and Risks:
- NASH is present in approximately 25% of individuals with NAFLD at any given time.
- Cirrhosis develops in about 6% of individuals with NAFLD.
- The risk for advanced liver fibrosis is highest in individuals with NASH who are aged >45-50 years, overweight/obese, or have type 2 diabetes.
- Once NAFLD-related cirrhosis develops, the annual incidence of primary liver cancer can be as high as 3%.
- Patients with NASH face a two- to threefold increased risk of developing metabolic syndrome.
Clinical Features
- Many cases are asymptomatic.
- Incidental findings include elevated serum aminotransferases and features of fatty liver on imaging.
- Obesity is prevalent in 50-90% of cases.
- Stigmata of chronic liver disease, such as spider angiomas, palmar erythema, or splenomegaly, may be observed.
- Complications of end-stage liver disease may include jaundice, ascites, and variceal hemorrhage.
Diagnosis
- Demonstration of Liver Fat:
- Use various diagnostic methods such as Ultrasound (USG), Fibroscan, and MRI (specifically MRI using proton density fat fraction [PDFF]).
- Evaluate Liver Function Tests (LFT), where an AST:ALT ratio less than 1 is indicative of nonalcoholic fatty liver disease.
- Liver biopsy may be performed for confirmation.
- Control of Alcohol Consumption:
- Ensure the absence of hazardous levels of alcohol consumption.
- Defined as one drink per day for women and no more than two drinks per day for men.
- One drink is equivalent to 10 g of ethanol, corresponding to one can of beer, 4 ounces of wine, or 1.5 ounces (one shot) of distilled spirits.
- Exclusion of Other Causes:
- Rule out other potential causes of liver fat accumulation.
Differential diagnosis-Causes of Hepatic Steatosis
- Causes of Liver Diseases Beyond NAFLD and Alcoholic Liver Disease:
- Alcoholic liver disease: Linked to excessive alcohol consumption.
- Hepatitis C (particularly genotype 3): A specific strain of hepatitis C virus affecting the liver.
- Inborn errors of metabolism: Genetic conditions like abetalipoproteinemia, cholesterol ester storage disease, galactosemia, glycogen storage disease, hereditary fructose intolerance, homocystinuria, systemic carnitine deficiency, tyrosinemia, Weber-Christian syndrome, Wilson's disease, and Wolman's disease impacting metabolism.
- Medications: Certain drugs like L-asparaginase, bleomycin, methotrexate, tetracycline, doxycycline, amiodarone, estrogens, glucocorticoids, HAART, tamoxifen, hydralazine.
- Miscellaneous Causes:
- Industrial exposure to chemicals.
- Inflammatory bowel diseases.
- Atrophy or undergrowth of the liver.
- Surgical procedures like biliopancreatic diversion, extensive small-bowel resection, gastric bypass, jejunoileal bypass.
- Specific conditions like Reye's syndrome, acute fatty liver of pregnancy, and HELLP syndrome (hemolytic anemia, elevated liver enzymes, low platelet count).
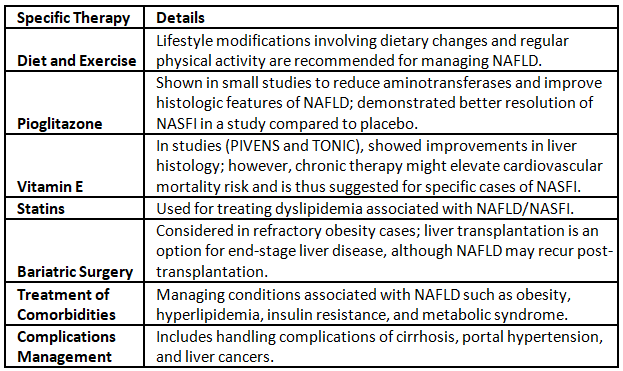
- Treatment for NAFLD:
- Currently, there are no FDA-approved therapies for NAFLD treatment.
Weight loss with altered bowel habits
- Intestinal Tuberculosis: Gradual weight loss and altered bowel habits may be indicative of intestinal tuberculosis.
- Carcinoma Colon (Gastrointestinal Malignancies): Colon cancer or other gastrointestinal malignancies could be considered when there is a gradual loss of weight accompanied by altered bowel habits.
- Irritable Bowel Syndrome (IBS): Irritable bowel syndrome is a potential cause for weight loss and changes in bowel habits, particularly if there are no structural abnormalities.
- Inflammatory Bowel Disease (IBD): Conditions such as Crohn's disease or ulcerative colitis, falling under inflammatory bowel disease, might manifest with weight loss and altered bowel patterns.
- Diverticulitis: The presence of diverticula in the colon, especially if inflamed (diverticulitis), can lead to weight loss and changes in bowel habits.
- HIV/AIDS: Gradual weight loss and gastrointestinal symptoms may be linked to HIV/AIDS, suggesting the need to consider this viral infection.
- Hyperthyroidism: Overactive thyroid (hyperthyroidism) can contribute to weight loss and disruptions in bowel movements.
- Psychiatric Causes: Psychological factors may lead to weight loss and alterations in bowel habits, emphasizing the importance of considering mental health in the differential diagnosis.
- Malabsorption Syndromes: Various malabsorption disorders such as celiac disease, tropical sprue, and Whipple disease may result in weight loss and changes in bowel habits due to impaired nutrient absorption.
The phrase "change in bowel habits" is intentionally broad and can encompass various alterations such as shifts in frequency, consistency (diarrhea or constipation), or even changes in stool size. While colon cancer might be one reason behind these alterations, it's clear that numerous other factors could lead to similar changes in bowel patterns.
Malabsorption syndromes-Classification
- Pancreatic Insufficiency: Insufficient pancreatic function leading to malabsorption.
- Cystic Fibrosis: A genetic disorder causing thickened mucus, affecting various organs, including the pancreas.
- Parenchymal Liver Disease: Liver damage affecting the absorption of nutrients.
- Drug-Induced Malabsorption: Medications causing malabsorption issues.
- Bacterial Overgrowth Syndromes: Overgrowth of bacteria in the small intestine leading to malabsorption.
- Crohn's Disease: Inflammatory bowel disease affecting the digestive tract.
- Intestinal Resection or Celiac Disease: Surgical removal of part of the intestine or an autoimmune reaction to gluten.
- Tropical Sprue: Chronic malabsorption disorder in tropical regions.
- Whipple's Disease: Rare bacterial infection affecting various systems, including the digestive tract.
- Folate and Vitamin B12 Deficiency: Inadequate levels of these essential nutrients leading to malabsorption.
- GVHD (Graft-Versus-Host Disease): Complication post organ transplant causing malabsorption.
- Amyloidosis: Accumulation of abnormal proteins affecting various organs, including the digestive system.
- Intestinal Lymphoma: Cancer affecting the lymphatic system in the intestine.
- Abetalipoproteinemia: Genetic disorder affecting fat absorption.
- Cystinuria: Inherited disorder causing the accumulation of amino acid cystine.
- Hartnup Disease: Genetic disorder affecting the absorption of certain amino acids.
- Diabetes: Metabolic disorder affecting glucose regulation and absorption.
- Hypoparathyroidism: Insufficient parathyroid hormone affecting calcium absorption.
- Hyperthyroidism: Overactive thyroid affecting metabolism and nutrient absorption.
- Carcinoid Syndrome: Tumors producing hormones affecting the digestive system.
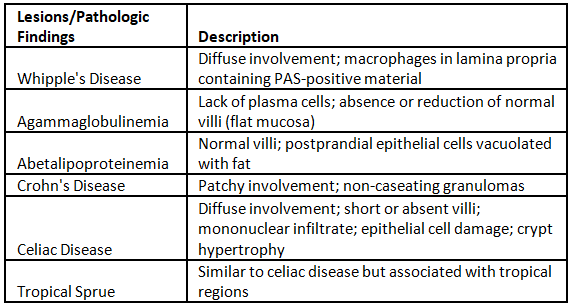
Malabsorption syndromes-Small intestinal mucosal biopsies
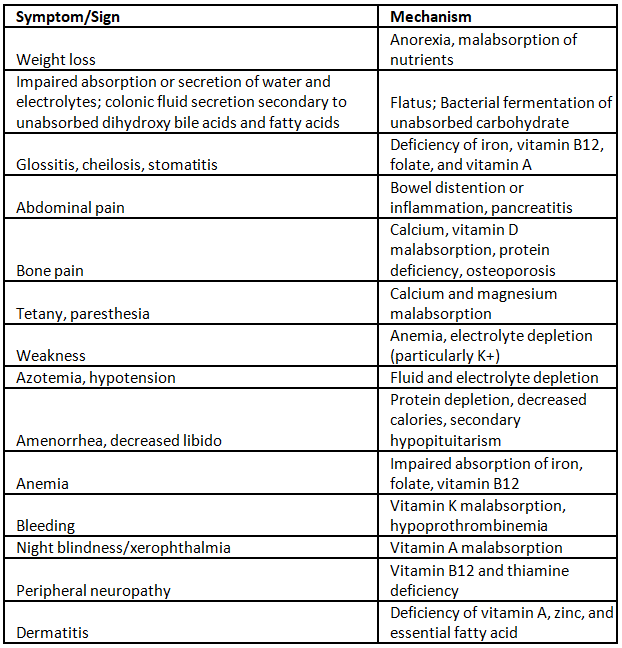
Malabsorption syndromes-ClinicaI manifestations
|
7 videos|236 docs
|
FAQs on Nonalcoholic Fatty Liver Diseases and Nonalcoholic Steatohepatitis (NAFLD/NASH) - Medical Science Optional Notes for UPSC
| 1. What is epidemiology? |  |
| 2. What is the pathogenesis of hepatic steatosis? |  |
| 3. What are the causes of hepatic steatosis? |  |
| 4. What are malabsorption syndromes? |  |
| 5. What are the clinical manifestations of malabsorption syndromes? |  |




















