Liver Abscess | Medical Science Optional Notes for UPSC PDF Download
| Table of contents |

|
| Liver Abscess-Etiology |

|
| Liver abscess-Clinical presentation |

|
| Liver abscess-investigations |

|
| Pyogenic vs amoebic liver abscess |

|
| Liver abscess-Repeats |

|
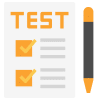
Liver Abscess-Etiology
- Pyogenic Liver Abscess (80% of cases):
- Predominantly caused by polymicrobial infections, with E. coli being the most common causative organism.
- K. pneumoniae is the second most common pathogen.
- Other bacteria contributing to the infection include Enterococci, Streptococci, Staphylococcus aureus, Proteus vulgaris, and anaerobes.
- Non-Pyogenic Liver Abscess:
- Fungal Infection (<10% of cases): Candida species are the predominant causative agents.
- Amebic Liver Abscess (<10% of cases): Entamoeba histolytica is the primary organism responsible for the infection.
Liver abscess-Clinical presentation
- Classic Triad of Pyogenic Liver Abscess:
- Fever (with or without chills and rigors).
- Malaise.
- Right upper quadrant pain.
- Other Symptoms:
- Anorexia and weight loss.
- Nausea and vomiting.
- Symptoms of diaphragmatic irritation.
- Physical Examination:
- Jaundice.
- Tender hepatomegaly.
- Intercostal tenderness.
- Epigastric tenderness.
- Decreased breath sounds in the right lower lobe of the lung.
- Features of sepsis.
- Note: The symptoms of pyogenic liver abscess are often non-specific, including fever, weight loss, and others.
Liver abscess-investigations
Laboratory Tests
- Complete Blood Count:
- Neutrophilic leukocytosis.
- Normocytic normochromic anemia.
- Liver Function Tests and Enzymes:
- Increased alkaline phosphatase (90%).
- Elevated AST and ALT.
- Hypoalbuminemia.
- Hyperbilirubinemia.
- Inflammatory Markers:
- Increased ESR and CRP.
- Blood Culture:
- Positive in approximately 50% of cases.
Imaging
- Abdominal imaging is confirmatory for pyogenic liver abscess.
- Abdominal Ultrasound (US):
- Solitary/multiple, poorly demarcated, fluid-filled, round hypoechoic lesion(s) within the hepatic parenchyma with surrounding edema and hyperemia.
- Abdominal CT Scan:
- Similar findings to abdominal ultrasound; peripheral rim enhancement is observed with IV contrast administration.
Percutaneous Aspiration and Culture of the Aspirate
- Both diagnostic and therapeutic (refer to the "Treatment" section below).
- Performed under US or CT guidance.
- Aspirated material is cultured to determine the organism and its antibiotic-susceptibility profile.
Liver abscess-Differential diagnosis
Pyogenic Liver Abscesses Need Differentiation from Other Space-Occupying Lesions of the Liver:
- Amebic Liver Abscess: Amebic liver abscess is one of the conditions requiring differentiation.
- Hepatic Echinococcosis (Hydatid Cyst of the Liver): Hepatic echinococcosis, specifically hydatid cysts of the liver, is another entity that needs to be distinguished.
- Hepatic Cysts: Simple hepatic cysts should be considered in the differential diagnosis.
- Benign Liver Tumors: Various benign liver tumors may present as space-occupying lesions and need to be differentiated.
- Hepatocellular Carcinoma: Hepatocellular carcinoma is a malignant liver tumor that requires consideration in the differential diagnosis.
- Liver Metastases: Metastatic lesions in the liver, originating from other primary sites, should also be distinguished from pyogenic liver abscesses.
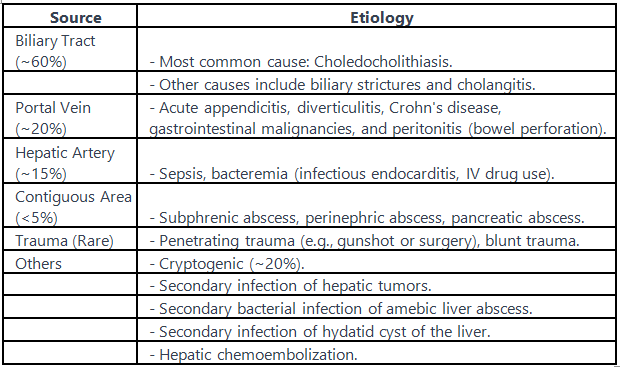
Liver abscess-Treatment
- Treatment Approach for Pyogenic Liver Abscesses: Pyogenic liver abscesses are typically managed with a combination of intravenous (IV) antibiotics and percutaneous drainage. Surgical drainage may be necessary in some cases.
- Antibiotics:
- Antibiotics are recommended for all cases.
- Broad-spectrum IV antibiotics include ampicillin + sulbactam, piperacillin + tazobactam, or a 3rd generation cephalosporin + metronidazole until antibiotic susceptibility is known.
- Drainage of the Abscess Cavity:
- Percutaneous drainage or needle aspiration is indicated for nearly all pyogenic liver abscess cases.
- For solitary abscess:
- Small abscesses (<5 cm) may be managed with percutaneous needle aspiration.
- Large abscesses (>5 cm) may require percutaneous drainage with intracavitary catheter placement.
- If percutaneous drainage/aspiration is unsuccessful, a second attempt can be made before considering surgical drainage.
- Indications for Surgical Drainage (Open/Laparoscopic):
- Multiple or loculated abscesses.
- Deep-seated abscess not amenable to percutaneous drainage.
- Ruptured abscess.
- Thick viscous pus that cannot be drained percutaneously.
- Underlying diseases requiring surgical intervention (e.g., choledocholithiasis, appendicitis, etc.).
- Contraindications: Coagulopathy (e.g., international normalized ratio (INR) > 1.5; thrombocytopenia due to sepsis).
- Considerations: The underlying etiology (e.g., choledocholithiasis, biliary stricture) should be addressed to prevent recurrent pyogenic liver abscesses.
Liver abscess-Complications
Complications of Liver Abscess:
- Rupture: Rupture can lead to various complications.
- Into the Abdomen (Peritonitis): Rupture into the abdomen can result in peritonitis.
- Into the Chest (Empyema): Rupture into the chest may lead to empyema.
- Into the Retroperitoneum (Retroperitoneal Abscess): Rupture into the retroperitoneum can cause the formation of a retroperitoneal abscess.
- Sepsis: Systemic infection (sepsis) is a potential complication.
- Pneumonia: Pneumonia can occur as a consequence.
- Pleural Effusion: Pleural effusion is another possible complication.
Poor Prognostic Factors:
- Certain factors indicate a less favorable prognosis.
- Pyogenic Abscess with Sepsis: Presence of sepsis in pyogenic abscess.
- Advanced Age (>70 Years): Older age, specifically over 70 years.
- Multiple Abscesses: The presence of multiple abscesses.
- Polymicrobial Infection; Anaerobic Infection: Infection involving multiple organisms or anaerobic bacteria.
- Immunosuppression (e.g., Malignancy, Diabetes): Weakened immune system due to conditions like malignancy or diabetes.
- Need for Surgical Drainage: The necessity for surgical drainage is also considered a poor prognostic factor.
 |
Download the notes
Liver Abscess
|
Download as PDF |
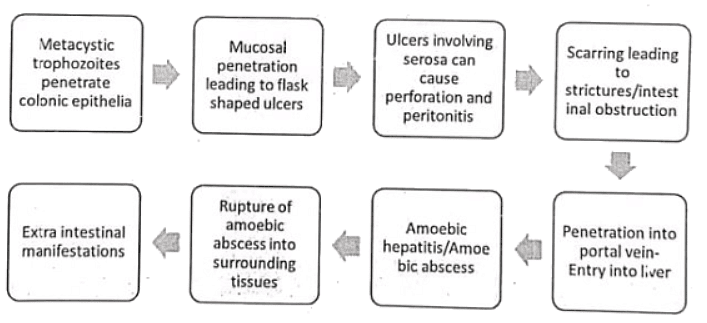
Pathogenesis of Amoebic liver abscess
Clinical features of Amoebic liver abscess
Intestinal Amebiasis (Dysentery):
- Loose stools with mucus and bright red blood.
- Symptoms include painful defecation, tenesmus, abdominal pain, cramps, weight loss, and anorexia.
- Fever occurs in 10-30% of cases, with possible systemic symptoms like fatigue.
- High risk of recurrence, often through self-inoculation (hand to mouth).
- A chronic form resembling inflammatory bowel disease is also possible.
Extraintestinal Amebiasis:
- Symptoms typically have an acute onset; subacute courses are rare.
- In 95% of cases, manifests as amebic liver abscess, usually a solitary abscess in the right lobe.
- Fever is present in 85-90% of cases (compared to amebic dysentery).
- Right upper quadrant pain or pressure sensation is common.
- Chest pain and pleuralgia may also occur.
- Diarrhea precedes only about a third of all cases of amebic liver abscess.
- In 5% of cases, abscesses may occur in other organs, especially the lungs, and in rare cases, the brain, with accompanying organ-specific symptoms.
- Diarrhea precedes only about a third of all cases of amebic liver abscess.
Management of Amoebic liver abscess
- Diagnosis:
- Liver function tests may exhibit mild abnormalities, with uncommon occurrences of hyperbilirubinemia.
- CT scans, more than ultrasounds, are the primary investigative tools.
- Confirmation of diagnosis involves serological tests (enzyme immunoassay) for antiamoebic antibodies.
- Cultures of amoebic abscesses usually yield negative results.
- Treatment:
- Invasive amebiasis is addressed with a nitroimidazole such as metronidazole or tinidazole, followed by a luminal amebicide like paromomycin.
- Indications for percutaneous aspiration in amebic liver abscess include:
- Large abscesses (>5 cm).
- Lack of response to medical therapy within 5 days.
- Suspected superinfection.
- Abscesses of the left lobe of the liver at risk for rupture into the pericardium.
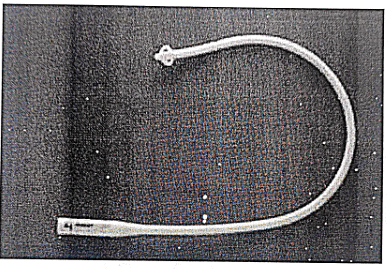
- Malecot Catheter:
- Utilized in draining amoebic liver abscesses.
- It is a self-retaining urinary catheter with an umbrella or flower tip.
- The catheter contains sulfur, making it radioopaque.
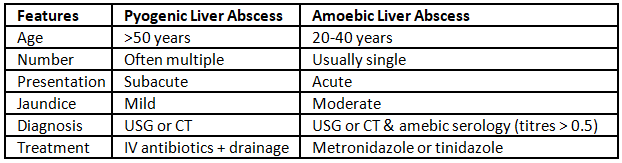
Pyogenic vs amoebic liver abscess
Liver abscess-Repeats
Q1: What is an abscess? Describe the method of draining a deep abscess by Hilton's method. (1995)
Q2: Describe the clinical features of amoebic abscess liver and its management. (1995)
Q3: Discuss pathogenesis and lab diagnosis of amoebic liver abscess. (1998)
Q4: What are the causes of liver abscess? Discuss their clinical presentation. How will you investigate and manage? (2006)
Q5: Enumerate the complications of liver abscess. How would you manage a 40-year old diabetic with suspected liver abscess in left lobe of liver? (2011)
Q6: What are the mode of infection, clinical presentation and complications of amoebic liver abscess? Briefly outline the management of patients with amoebic liver abscess including surgical intervention. (2013)
|
7 videos|219 docs
|
FAQs on Liver Abscess - Medical Science Optional Notes for UPSC
| 1. What is the etiology of liver abscess? |  |
| 2. What are the clinical presentations of liver abscess? |  |
| 3. What investigations are conducted for liver abscess? |  |
| 4. What are the differences between pyogenic and amoebic liver abscess? |  |
| 5. Can liver abscess recur? |  |