NRHM & RMNCH-A: Preventive medicine in Obstetrics and Pediatrics | Medical Science Optional Notes for UPSC PDF Download
National Health Mission (2013)
- The Ministry of Health and Family Welfare is implementing various schemes and programmes and national initiatives to provide universal access to quality health care.
- NRHM (National Rural Health Mission) and NUHM (National Urban Health Mission) are two submissions of National Health Mission.
Main Components
- Health system strengthening
- RMNCH-A (Reproductive-Maternal-Newborn-Child and Adolescent health)
- Control of communicable and non-communicable diseases
NRHM Strategies
Core Strategies
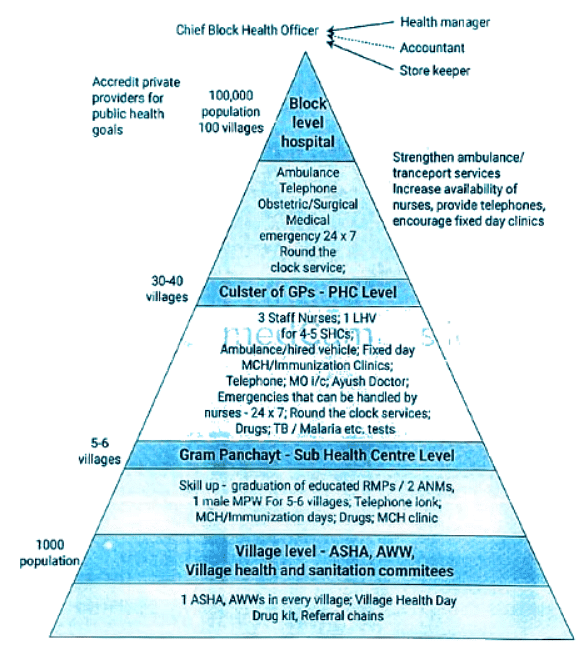
- Build and enhance the capabilities of Panchayat Raj Institutions (PRIs) to take responsibility for, control, and manage public health services.
- Encourage improved healthcare accessibility at the household level by empowering female health activists (ASHA workers).
- Establish a Health Plan for each village through the Village Health Committee of the Panchayat.
- Reinforce sub-centers by providing untied funds for local planning and action, along with an increased number of Multi-Purpose Workers (MPWs).
- Strengthen existing Primary Health Centers (PHCs) and Community Health Centers (CHCs), aiming for a 30-50 bedded CHC per lakh population to meet specified standards in personnel, equipment, and management.
- Develop and implement an inter-sectoral District Health Plan, incorporating aspects such as drinking water, sanitation, hygiene, and nutrition, through the District Health Mission.
- Integrate vertical Health and Family Welfare programs at the National, State, Block, and District levels.
- Provide technical support to National, State, and District Health Missions for effective Public Health Management.
- Reinforce capacities for data collection, assessment, and review to facilitate evidence-based planning, monitoring, and supervision.
- Formulate transparent policies for the deployment and career development of human resources in health.
- Develop capacities for preventive healthcare at all levels to encourage healthy lifestyles and reduce the consumption of tobacco and alcohol.
- Encourage the non-profit sector, especially in under-served areas.
NRHM Supplementary Strategies
- Regulate the private sector, including informal rural practitioners, to guarantee the availability of quality services to citizens at an affordable cost.
- Foster Public Private Partnerships to attain public health objectives.
- Integrate AVUSH (revitalizing local health traditions) into mainstream healthcare.
- Revise medical education to address rural health issues, including the regulation of medical care and medical ethics.
- Establish efficient and sustainable risk pooling and social health insurance systems to offer health security to the economically disadvantaged, ensuring accessible, affordable, accountable, and high-quality hospital care.
NRHM Initiatives
Major Initiatives
- Selection of ASHA (Accredited Social Health Activist).
- Establishment of Rogi Kalyan Samiti (Patient Welfare Committee/Hospital Management Society).
- Allocation of untied grants to sub-centers (SCs).
- Formation of Village Health Sanitation and Nutrition Committee (VHSNC).
- Implementation of Janani Suraksha Yojana (JSY).
- Introduction of Janani Shishu Suraksha Karyakram (JSSK).
- Deployment of National Mobile Medical Units (NMMUs).
- Launching National Ambulance Services.
- Implementation of Web-enabled Mother and Child Tracking System (MCTS).
New Initiatives (Decisions of Mission Steering Group: 2011)
- Home delivery of contraceptives facilitated by ASHA.
- Involvement of ASHA in Home-Based Newborn Care.
- Menstrual Hygiene scheme with modifications.
- Adoption of a differential financial approach based on the case load in a health facility.
- Mainstreaming of AYUSH (Ayurveda, Yoga & Naturopathy, Unani, Siddha, and Homeopathy) under NRHM.
- Implementation of Rasthriya Bal Swasthya Karyakram (RBSK).
- Introduction of Rasthriya Kishor Swasthya Karyakram (RKSK).
- Establishment of Mother and Child Health Wings (MCH Wings).
- Provision of free drugs and free diagnostic services.
- Launch of the National IRON + Initiative.
- Implementation of the RMNCH+A approach (Reproductive, Maternal, Newborn, Child, and Adolescent Health).
- Focused support for high-demand health facilities through Delivery Points (DPs).
- Implementation of Universal Health Coverage (UHC).
Infrastructure of NRHM
RMNCH+A Goals and Targets
RMNCH+A Strategy is based on provision of comprehensive care through the five pillars, or thematic areas, of reproductive, maternal, neonatal, child, and adolescent health, and is guided by central tenets of equity, universal care, entitlement, and accountability.
The "plus" within the strategy focusses on:
- Including adolescence for the first time as a distinct life stage
- Linking maternal and child health to reproductive health, family planning, adolescent health, HIV, gender, preconception and prenatal diagnostic techniques
- Linking home and community-based services to facility based care
- Ensuring linkages, referrals, and counter-referrals between and among health facilities at primary (primary health centre), secondary (community health centre),and tertiary levels (district hospital)
Three Goals
- Achieve a reduction in Infant Mortality Rate (IMR) to 25 per 1,000 live births by the year 2017.
- Attain a reduction in Maternal Mortality Ratio (MMR) to 100 per 100,000 live births by the year 2017.
- Achieve a reduction in Total Fertility Rate (TFR) to 2.1 by the year 2017.
Coverage Targets for Key RMNCH+A Interventions for 2017
- Double the number of facilities equipped for perinatal care (designated as 'delivery points').
- Increase the proportion of all births in government and accredited private institutions by an annual rate of 5.6%, starting from the baseline of 61% (SRS 2010).
- Raise the proportion of pregnant women receiving antenatal care by an annual rate of 6%, starting from the baseline of 53% (CES 2009).
- Increase the proportion of mothers and newborns receiving postnatal care by an annual rate of 7.5%, starting from the baseline of 45% (CES 2009).
- Increase the proportion of deliveries conducted by skilled birth attendants by an annual rate of 2%, starting from the baseline of 76% (CES 2009).
- Enhance exclusive breastfeeding rates by an annual rate of 9.6%, starting from the baseline of 35% (CES 2009).
- Reduce the prevalence of underweight children under five at an annual rate of 5.5%, starting from the baseline of 45% (NFHS-3).
- Increase the coverage of three doses of combined diphtheria-tetanus-pertussis (DTP3) for children aged 12-23 months by an annual rate of 3.5%, starting from the baseline of 7% (CES 2009).
- Increase Oral Rehydration Solution (ORS) use in under-five children with diarrhea by an annual rate of 7.2%, starting from the baseline of 43% (CES 2009).
- Reduce the unmet need for family planning methods among eligible couples, both married and unmarried, by an annual rate from the baseline of 21% (DLHS 3).
- Increase the met need for modern family planning methods among eligible couples by an annual rate of 4.5%, starting from the baseline of 47% (DLHS 3).
- Decrease the prevalence of anemia in adolescent girls and boys (15-19 years) by an annual rate of 6%, starting from the baseline of 56% and 30%, respectively (NFHS-3).
- Decrease the proportion of total fertility contributed by adolescents (15-19 years) by an annual rate of 3.8%, starting from the baseline of 16% (NFHS-3).
- Improve the child sex ratio in the 0-6 years age group by an annual rate of 0.6%, starting from the baseline of 914 (Census 2011).
Janani Suraksha Yojana (JSY)
Objective:
- Launched on April 12, 2005, as a modification of the national maternity benefit scheme.
- Aims to reduce maternal mortality by encouraging pregnant women, especially those from below poverty line (BPL) families, to deliver in government health facilities, emphasizing institutional care.
Salient Features:
- A 100% centrally sponsored scheme.
- States are categorized into low performing states (LPS) and high performing states (HPS) based on institutional delivery rates.
- Low Performing States (LPS) include Uttar Pradesh, Uttarakhand, Madhya Pradesh, Jharkhand, Bihar, Rajasthan, Chhattisgarh, Odisha, Assam, and Jammu and Kashmir, while the remaining states are considered High Performing States.
- Cash benefits are provided to all BPL women, both rural and urban, with direct transfer to the Aadhar-linked bank accounts of eligible pregnant women.
- Eligibility for cash assistance differs between LPS and HPS:
- In LPS: All women, including those from SC, ST families.
- In HPS: Limited to below poverty line women, and SC, ST pregnant women.
- Cash benefits for institutional deliveries apply to the first two live births in case of HPL, with the age and birth order restrictions lifted in LPS.
- For home deliveries, all BPL women in rural and urban areas receive cash assistance (Rs.500 per delivery) regardless of age and number of children.
Role of ASHA:
- ASHA serves as a link worker connecting poor pregnant women with public sector health institutions in LPS.
- Responsible for facilitating access to institutional antenatal and postnatal care.
- Escorts pregnant women to health centers.
- Receives money after a postnatal visit, following the child's immunization with BCG.
Packages: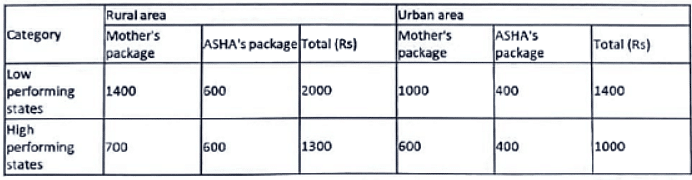
Janani Shishu Suraksha Karyakram (JSSK)
Launched on June 1, 2011, JSSK is a fresh national initiative aimed at enhancing health facilities for women and children. Under this program, every pregnant woman delivering in public health institutions is entitled to completely free delivery, including free cesarean sections.
The entitlements encompass: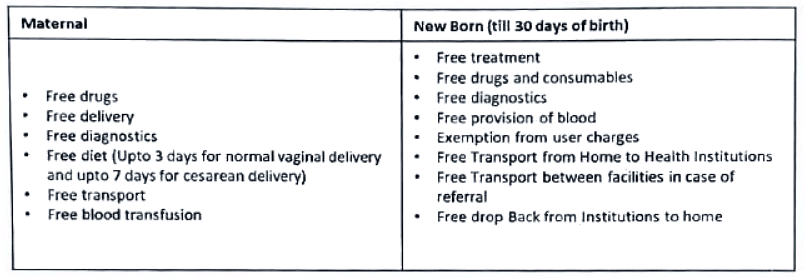 The scheme has now been extended to cover the complications during ANC, PNC and also sick infants.
The scheme has now been extended to cover the complications during ANC, PNC and also sick infants.
Vandemataram Scheme
- Voluntary scheme to provide safe motherhood services
- Any obstetric and gynaecology specialist, maternity home, nursing home, lady doctor/mbbs doctor can be a part of it
- After enrollment, doctors will display Vandemataram logo at their clinic.
- Respective district medical officer will provide these clinics/doctors with Iron-Folic acid tablets, oral pills, TT injections etc. for free distribution to the beneficiaries.
- Vandematarm cards will be provided to their patients by respective doctors/clinics. In case of referral to government hospitals, upon showingthis card due care is provided.
Rasthriya Bal Swasthya Karyakram (RBSK)
Overview:
Launched in February 2013, Rastriya Bal Swasthya Karyakram (RBSK) is a crucial initiative designed to identify and intervene early for children aged birth to 18 years, covering four domains known as the 4 'D's, which include:
- Defects at birth
- Deficiencies
- Diseases
- Development delays, including disabilities.
Key Points:
- RBSK encompasses the screening and early intervention for 30 identified health conditions, ensuring free treatment and management.
Defects at Birth:
- Neural tube defect
- Down's syndrome
- Cleft lip and cleft palate
- Club foot
- Developmental dysplasia of the hip
- Congenital cataract
- Congenital deafness
- Congenital heart diseases
- Retinopathy of prematurity
Deficiencies:
- Anemia
- Vitamin A deficiency
- Vitamin D deficiency
- Severe acute malnutrition
- Goitre
Childhood Diseases:
- Skin conditions (fungal infection, eczema, scabies)
- Otitis media
- Rheumatic heart disease
- Reactive airway disease
- Dental caries
- Convulsive disorders
Developmental Delays and Disabilities:
- Vision impairment
- Hearing impairment
- Neuro-motor impairment
- Motor delay
- Cognitive delay
- Language delay
- Behaviour disorder (Autism)
- Learning disorder
- ADHD (Attention Deficit Hyperactivity Disorder)
- Optional (Congenital hypothyroidism, sickle cell anemia, Beta Thalessemia)
Rasthriya Bal Swasthya Karyakram (RBSK)- Programme implementation: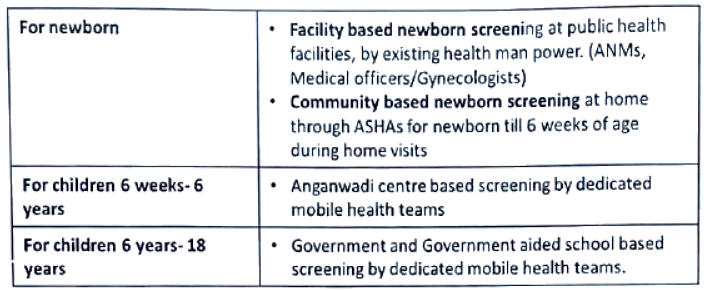
Navjat Shishu Suraksha Karyakram (NSSK)
- NSSK is a program designed to train health personnel in basic newborn care and resuscitation.
- The primary objective is to ensure the presence of a trained health professional in basic newborn care and resuscitation at every delivery point.
- The program addresses key aspects including:
- Prevention of hypothermia
- Prevention of infection
- Early initiation of breastfeeding
- Basic newborn resuscitation
- The training duration is two days, and it is anticipated to contribute significantly to the reduction of neonatal mortality in the country.
Menstrual Hygiene Scheme
- The Ministry of Health and Family Welfare has initiated a scheme to promote menstrual hygiene among rural adolescent girls aged 10-19 years.
- The program aims to provide comprehensive knowledge about menstrual hygiene and ensure access to high-quality sanitary napkins along with safe disposal methods.
Key activities and objectives include:
- Community-based health education and outreach targeting the specified age group.
- Ensuring a consistent supply of sanitary napkins to adolescents.
- Sourcing and procurement of sanitary napkins.
- Storage and distribution of sanitary napkins to adolescent girls.
- Training Accredited Social Health Activists (ASHA) and nodal teachers in menstrual health.
- Ensuring the safe disposal of sanitary napkins.
The overarching framework for scheme implementation in the state involves:
- Accredited Social Health Activists (ASHAs) selling napkins at Rs. 6 for a pack of six to adolescent girls through door-to-door sales, school, and Anganwadi Centres.
- ASHAs receiving Rs. 1 as an incentive for each pack sold, in addition to a free pack of sanitary napkins each month.
- Utilizing the funds from sales for transportation, storage costs, and providing Rs. 50 as an incentive to ASHAs for conducting monthly health meetings with adolescent girls.
- The remaining funds to be recouped to the State Health Society Account for procurement in the subsequent year.
Mission Parivar Vikas
- The declaration for Mission Parivar Vikas was made on September 26, 2016.
- Launched in 146 high Total Fertility Rate (TFR) districts, this program aims to accelerate the utilization and awareness of family planning methods.
- State and district fact sheets provide a baseline and roadmap for future work by highlighting current indicators and trends in these districts.
- The mission operates under a five-pronged strategy, encompassing:
a. Delivering assured services.
b. Building additional capacity/human resources for enhanced service delivery.
c. Ensuring commodity security.
d. Implementing new promotional schemes.
e. Creating an enabling environment. - The Health & Family Welfare Ministry is responsible for overseeing all activities and decisions related to Mission Parivar Vikas.
- The target is to achieve an ideal Total Fertility Rate (TFR) as all seven states and 145 districts have a fertility rate exceeding 4%. These areas constitute 44% of the total population, and the scheme aims to lower the fertility rate to 2.1% by 2025, following the guidelines of the program.
SUMAN Scheme
Introduction:
- The Surakshit Matritva Aashwasan initiative, known as the SUMAN scheme, is designed to offer dignified and high-quality healthcare at no cost to every woman and newborn who visits a public health facility.
Significance of the SUMAN Scheme:
- The primary goal of the SUMAN scheme is to reduce maternal and infant mortality rates across the nation and eliminate all preventable maternal and newborn deaths.
- The scheme is committed to providing a positive and stress-free birth experience for both the mother and the newborn.
Key Objectives:
- The government emphasizes dignified care, including early initiation and support for breastfeeding.
- Free and zero-expense services are provided for sick newborns and neonates.
- Zero-dose vaccination is also covered under the scheme.
Positive Birth Experience:
- One of the core aims of the SUMAN scheme is to ensure a positive birth experience for both the mother and the infant.
Roles and Responsibilities of ASHA (Accredited Social Health Activist)
Profile of ASHA:
- ASHA is a trained woman volunteer residing in the village, married/widow/divorced, with formal education up to the 8th standard, preferably aged between 25-45 years.
- The standard guideline is one ASHA per 1000 population.
Health Awareness and Information:
- ASHA takes initiatives to create awareness and provide information to the community on health determinants such as nutrition, basic sanitation, hygienic practices, healthy living, working conditions, existing health services, and the importance of timely utilization of health and family welfare services.
Counseling Services:
- ASHA counsels women on birth preparedness, emphasizes the significance of safe delivery, advocates for proper breastfeeding and complementary feeding, promotes immunization, contraception, and educates on the prevention of common infections, including reproductive tract infections and sexually transmitted infections. She also provides guidance on caring for young children.
Community Mobilization:
- ASHA mobilizes the community and facilitates access to health and health-related services available at anganwadi/sub-centre/primary health centers. This includes services like immunization, antenatal check-ups, postnatal check-ups, supplementary nutrition, and sanitation.
Village Health Planning:
- ASHA collaborates with the village health and sanitation committee of the gram panchayat to develop a comprehensive village health plan.
Escort Services:
- ASHA arranges escort/accompaniment for pregnant women and children requiring treatment or admission to the nearest pre-identified health facility.
Primary Medical Care:
- ASHA provides primary medical care for minor ailments such as diarrhea, fevers, and offers first aid for minor injuries. She is also a provider of directly observed treatment short-course (DOTS) under the revised national tuberculosis control program.
Depot Holder for Essential Provisions:
- ASHA acts as a depot holder for essential provisions available to every habitation, including oral rehydration therapy, iron-folic acid tablets, chloroquine, disposable delivery kits, oral pills, condoms, etc. Each ASHA is provided with a drug kit based on recommendations from the government.
Reporting Births and Deaths:
- ASHA reports births and deaths in her village and informs about any unusual health problems or disease outbreaks in the community to the sub-centre/primary health center.
Promotion of Sanitation:
- ASHA promotes the construction of household toilets under the total sanitation campaign.
Formation and Promotion of Women's Health Committees:
- ASHA actively participates in the formation and promotion of Mahila Arogya Samitis in her community.
Incentive System:
- In return for services rendered, ASHA receives a performance-based incentive.
Roles and Responsibilities of ASHA in Home Based Newborn Care (HBNC)
Overview:
- A new scheme has been initiated to incentivize ASHA for providing Home Based Newborn Care (HBNC).
Home Visits Schedule:
- ASHA is tasked with making visits to all newborns up to 42 days of life, following a specified schedule.
- For institutional delivery, there are six visits, while for home delivery, seven visits are scheduled. Additional visits are required for sick and small newborns.
Incentive Scheme:
- ASHA receives an incentive of Rs. 50 per home visit, with a total of Rs. 250 for five visits.
- The incentive is paid once after 45 days of delivery, subject to certain conditions:
- Recording the newborn's weight in the MCP card.
- Ensuring BCG, 1st dose of OPV, and DPT vaccinations.
- Confirming the safety of both the mother and the newborn until 42 days after delivery.
- Completion of the birth registration process.
Visit Schedule for Special Cases:
- Sick newborns discharged from SNCU or those born preterm or with low birth weight require additional visits.
- For SNCU discharge, the first home visit is within 24 hours of discharge, with subsequent visits following the HBNC schedule.
- LBW or preterm newborns not requiring SNCU admission have visits once every quarter starting from the 3rd month until one year of life.
Operational Guidelines:
- The "Home Based Newborn Care Operational Guideline-2011" was developed, published, and disseminated by the Child Health Division, MoHFW, GOI in 2011. This guideline serves as a comprehensive framework, providing guidance for a coherent HBNC strategy and acting as a reference tool for states to plan necessary interventions.
Roles and Responsibilities of ASHA in Home Based Newborn Care (HBNC)
Overview:
- The National Health Mission, under the Child Health division, MoHFW, has introduced the Home-Based Care for Young Child (HBYC) Program, extending the Home-Based Newborn Care (HBNC) initiative. This program aims to promote evidence-based interventions in four key domains: nutrition, health, childhood development, and WASH (Water, Sanitation, and Hygiene).
Operational Guidelines:
- An operational guideline for the Home-Based Care for Young Child (HBYC) program was released by the Hon'ble Prime Minister of India on April 14, 2018, in Chhattisgarh.
Additional Home Visits by ASHA:
- Under the HBYC program, ASHA will conduct five additional home visits, supported by Anganwadi workers.
- The home visits are scheduled on the 3rd, 6th, 9th, 12th, and 15th months to promote early initiation of breastfeeding, exclusive breastfeeding until 6 months, continued breastfeeding until the 2nd year of life, adequate complementary feeding, prevention of childhood pneumonia and diarrhea, and ensuring age-appropriate immunization and early childhood development.
Harmonization of Visits Schedule:
- The quarterly home visits schedule for low birth weight babies, SNCU & NRC discharges will be harmonized with the new HBYC schedule.
Incentive and Kit Provision:
- ASHAs will receive an incentive of Rs. 250 for completing five home visits under HBYC for each young child (Rs. 50 per visit) as per the recommended schedule.
- Additional commodities, including ORS packets and Iron Folic Acid syrup, will be provided in the kit.
 |
Download the notes
NRHM & RMNCH-A: Preventive medicine in Obstetrics and Pediatrics
|
Download as PDF |
PCPNDT ACT
PCPNDT Act (Pre-Conception & Pre-Natal Diagnostic Techniques Act, 1994 and Rules with Amendments):
Current Sex Ratio in India:
- As of 2019, the sex ratio in India is 107.48, indicating 107.48 males per 100 females. This translates to 930 females per 1000 males, with 48.20% of the population being female and 51.80% male.
Male Preference and Female Foeticide:
- Despite advancements in education, there is a persistent strong male preference, leading to the unfortunate practice of female foeticide. The use of scientific methods in determining the sex of the foetus, such as amniocentesis, chorion villus biopsy, and ultrasonography, has contributed to the increase in female foeticide.
Enactment of PCPNDT Act:
- To address the alarming issue of female foeticide, the Parliament enacted the Pre-Natal Diagnostic Techniques (Regulation and Prevention of Misuse) Act on September 20, 1994. The aim was to regulate the use of pre-natal diagnostic techniques for detecting genetic disorders, chromosomal abnormalities, and sex-linked disorders, preventing their misuse for pre-natal sex determination.
Implementation and Amendments:
- The Act came into force in 1996. However, during its implementation, certain inadequacies and practical difficulties were identified. Consequently, the PNDT Act underwent amendments to address these issues.
Amended Title:
- The amended Act is now titled "The Pre-conception and Pre-natal Diagnostic Techniques (Prohibition of Sex Selection) Act."
Objective of the Amended Act:
- The Act aims to prohibit sex selection before or after conception and regulate pre-natal diagnostic techniques. It focuses on detecting abnormalities, metabolic disorders, chromosomal abnormalities, congenital malformations, and sex-linked disorders. The primary goal is to prevent the misuse of these techniques for sex determination, specifically targeting female foeticide.
Comprehensive Legislation:
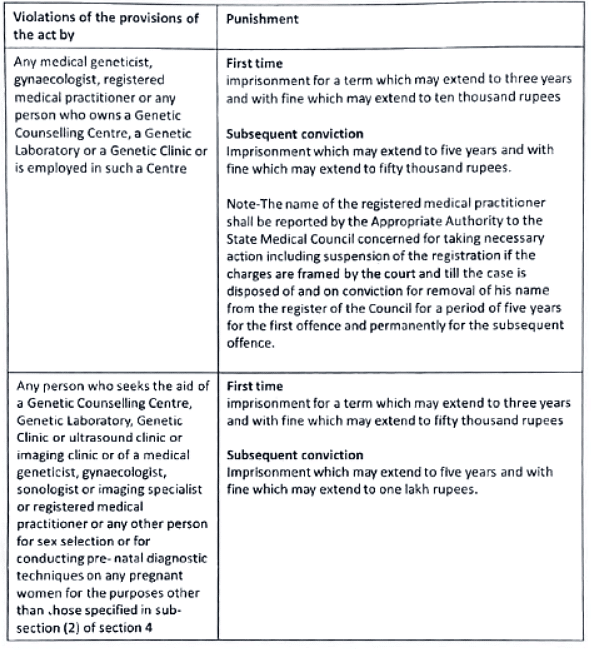
- The PCPNDT Act is a comprehensive piece of legislation that not only prohibits sex selection but also addresses the misuse of pre-natal diagnostic techniques. This includes provisions against advertisements related to sex determination techniques. The Act outlines specific punishments for any violation of its provisions.
The PCPNDT Act reflects the government's commitment to combating the issue of female foeticide by regulating and preventing the misuse of pre-natal diagnostic techniques.
PCPNDT ACT - Forms
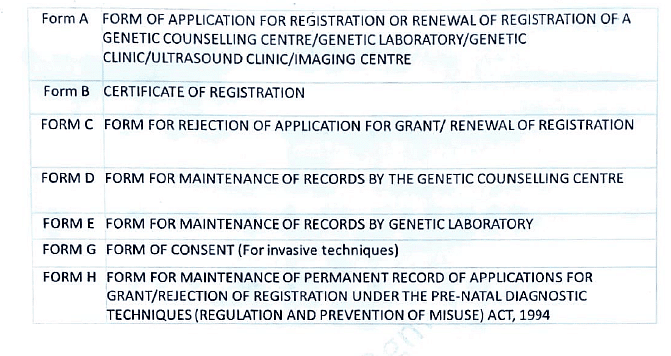
PCPNDT Act Forms: Form F
Declaration of Doctor/Person Conducting Ultrasonography/Image Scanning
- I, [Name of the person conducting ultrasonography/image scanning], declare that while conducting ultrasonography/image scanning on Ms. [Name of the pregnant woman], I have neither detected nor disclosed the sex of her foetus to anybody in any manner.
Name and Signature of the Person Conducting Ultrasonography/Image Scanning/Director or Owner of Genetic Clinic/Ultrasound Clinic/Imaging Center.
Important Note:
i. Ultrasound is not indicated/advised/performed to determine the sex of the foetus except for the diagnosis of sex-linked diseases such as Duchenne Muscular Dystrophy, Haemophilia A & B, etc.
ii. During pregnancy, Ultrasonography should only be performed when indicated.
The following is a representative list of indications for ultrasound during pregnancy:
- To diagnose intra-uterine and/or ectopic pregnancy and confirm viability.
- Estimation of gestational age (dating).
- Detection of the number of foetuses and their chorionicity.
- Suspected pregnancy with IUCD in-situ or suspected pregnancy following contraceptive failure/MTP failure.
- Vaginal bleeding/leaking.
- Follow-up of cases of abortion.
- Assessment of cervical canal and diameter of the internal os.
- Discrepancy between uterine size and period of amenorrhoea.
- Any suspected adnexal or uterine pathology/abnormality.
- Detection of chromosomal abnormalities, foetal structural defects, and other abnormalities and their follow-up.
- To evaluate foetal presentation and position.
- Assessment of liquor amnii.
- Preterm labour/preterm premature rupture of membranes.
- Evaluation of placental position, thickness, grading, and abnormalities (placenta praevia, retroplacental haemorrhage, abnormal adherence, etc.).
- Evaluation of umbilical cord - presentation, insertion, nuchal encirclement, the number of vessels, and the presence of a true knot.
- Evaluation of previous Caesarean Section scars.
- Evaluation of foetal growth parameters, foetal weight, and foetal well-being.
- Colour flow mapping and duplex Doppler studies.
- Ultrasound-guided procedures such as medical termination of pregnancy, external cephalic version, etc., and their follow-up.
- Adjunct to diagnostic and therapeutic invasive interventions such as chorionic villus sampling (CVS), amniocenteses, foetal blood sampling, foetal skin biopsy, amnio-infusion, intrauterine infusion, placement of shunts, etc.
- Observation of intra-partum events.
- Medical/surgical conditions complicating pregnancy.
- Research/scientific studies in recognized institutions.
PCPNDT ACT Offences and Penalties
Key Highlights of PCPNDT Act Compliance
- Doctor Qualification and Registration:
- All radiologists/sonologists/doctors utilizing USG machines must have their names entered in the PC-PNDT certificate or on a separate sheet displayed along with the PC-PNDT registration certificate.
- Qualification to perform ultrasound should align with their degree/diploma certificate.
- Record Maintenance:
- All records, including images, of patients must be maintained for a minimum of 2 years.
- In the case of any legal proceedings against the center, the relevant records should be retained until the case is disposed of.
- Mandatory Form F Filing:
- Form F filing is obligatory for all pregnant patients.
- The form should be complete and error-free, enabling authorities to contact the patient based on the information provided.
- All columns must be filled, and if any points are not applicable, write "NA" or "Not Applicable" against those columns—no blanks should be left.
- Proper maintenance of forms for easy accessibility when required.
Antenatal Care and Essential Investigations
Antenatal care involves systematic supervision of women during pregnancy, monitoring foetal growth, and ensuring the well-being of both mother and foetus. Proper check-ups are crucial for identifying complications such as anaemia, pre-eclampsia, and hypertension, enabling timely management through referral to appropriate facilities.
Antenatal Visit Schedule
- First Visit/Registration: Ideally within 12 weeks, as soon as pregnancy is suspected.
- Second Visit: Between 14 and 26 weeks.
- Third Visit: Between 28 and 34 weeks.
- Fourth Visit: Between 36 weeks and term.
Essential Components of Antenatal Check-ups:
- History Taking: Comprehensive patient history.
- Physical Examination: Measurement of weight, blood pressure, respiratory rate, and assessment for pallor and oedema.
- Abdominal Palpation: For foetal growth, foetal lie, and auscultation of foetal heart sounds.
Laboratory Investigations:
- Haemoglobin estimation.
- Urine tests for sugar and proteins.
Interventions and Counselling:
- Iron and folic acid supplementation as needed.
- Tetanus immunization.
- Nutrition, family planning, self-care, delivery, and parenthood guidance.
- Home visits by female health workers/trained personnel.
- Referral services when necessary.
- Informing women about government incentives, such as Janani Suraksha Yojana.
laboratory investigations
The following laboratory investigations are carried out at the facilities indicated below:
a. At the sub-centre:
- Pregnancy detection test.
- Haemoglobin examination.
- Urine test for presence of albumin and sugar
- Rapid malaria test.
b. At the PHC/CHC/FRU:
- Blood group, including Rh factor.
- VDRL/RPR.
- HIV testing.
- Rapid malaria test (if unavailable at SC).
- Blood sugar testing.
- HBSAG for hepatitis B infection.
Identification of At-Risk Infants
In communities or child health clinics with a large number of infants and children aged 1-5, it's essential to prioritize those "at-risk" to provide specialized and intensive care. This focus on at-risk infants significantly contributes to reducing perinatal, neonatal, and infant mortality rates.
The key criteria for identifying at-risk infants include:
- Birth Weight Less than 2.5 kg: Infants born with low birth weight need special attention.
- Twins: Multiple births, such as twins, require intensified care due to potential health complexities.
- Birth Order 5 and More: Higher birth order may increase the risk, demanding closer monitoring.
- Artificial Feeding: Infants reliant on artificial feeding may face additional challenges and require careful attention.
- Weight Below 70% of Expected Weight: Infants weighing less than 70% of the expected weight, indicating malnutrition (II and III degrees), need special care.
- Failure to Gain Weight During Three Successive Months: Infants who do not show weight gain over three consecutive months require intervention.
- Children with Protein-Energy Malnutrition (PEM) and Diarrhoea: Infants facing PEM or persistent diarrhoea are at higher risk and need targeted care.
- Working Mother/One Parent: Infants with mothers who work or have only one parent may require additional support due to potential caregiving challenges.
Antenatal Pediatrics: A Paradigm in Preventive Pediatrics
- Preventive pediatrics focuses on averting diseases and disabilities rather than curing them, encompassing both antenatal and postnatal aspects. Antenatal pediatrics, emerging in response to shifting healthcare needs, is integral to safeguarding maternal, perinatal, and neonatal health.
- Historically, antenatal care primarily aimed at preventing maternal mortality. Today, with maternal mortality reduced to approximately 0.2 per 1000 live births, the focus has expanded. Antenatal pediatrics now addresses perinatal mortality, morbidity prevention, and the well-being of the "foetus at risk."
- Advancements like amniocentesis, ultrasonography, cystoscopy, and chorion biopsy have revolutionized the diagnosis of congenital abnormalities and inborn errors of metabolism. Understanding that causation and prevention can occur in intra-uterine life has shifted the emphasis toward preventing disorders, giving rise to the concept of antenatal pediatrics.
- Antenatal care should ideally commence before conception, involving measures such as:
- Genetic Counselling for Prospective Parents: Providing guidance on hereditary factors and potential risks.
- Birth Spacing and Limitation: Encouraging intervals of 2-3 years between births for maternal and child health.
- Delaying First Pregnancy: Ensuring young women are physically and socially prepared for pregnancy.
- Ensuring Adequate Maternal Nutrition: Addressing nutritional needs to support both mother and foetus.
- Protection Against Intrauterine Infections: Implementing measures to shield the unborn from infections and adverse influences.
While resource limitations in developing countries like India may pose challenges, elements such as improving maternal nutrition, family planning, and counseling can significantly contribute to enhancing maternal and foetal health. Antenatal pediatrics stands as a crucial component in the broader spectrum of preventive pediatrics, emphasizing proactive measures to secure the well-being of both mother and child.
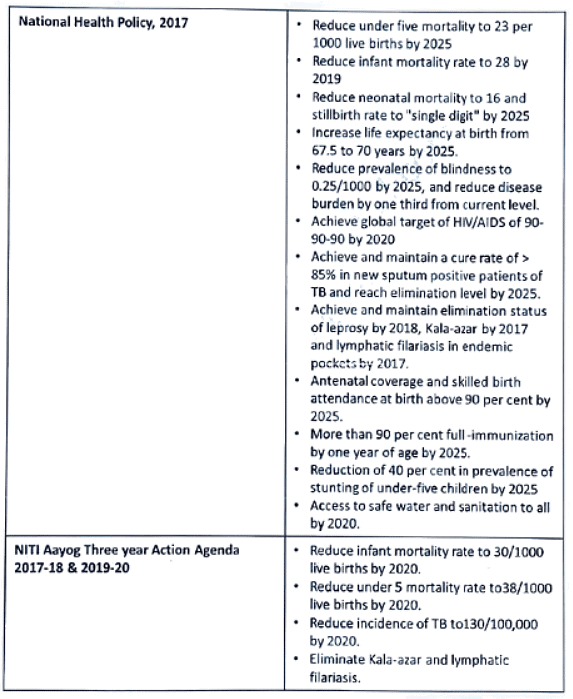
Child Health Goals and Targets in India
Goals and targets set by Government of India for child health under various national and international commitments are as follows: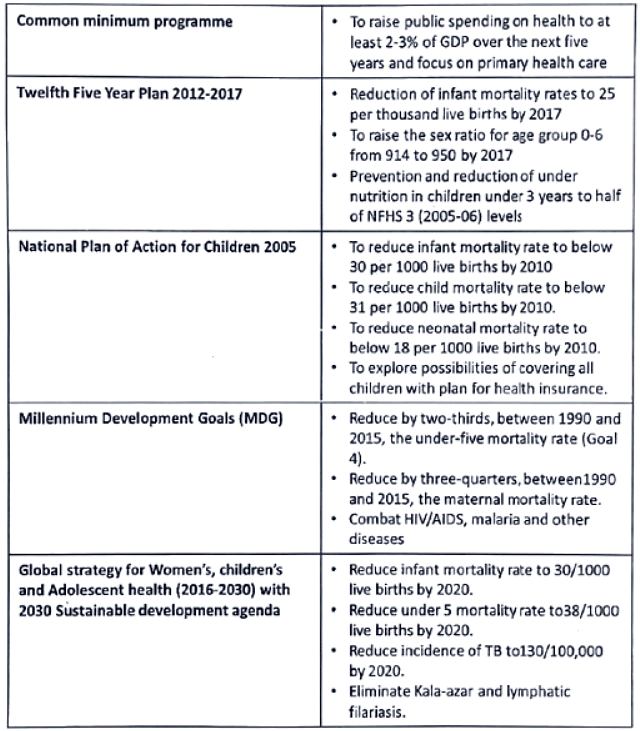
POCSO Act, 2012 (Protection of Children from Sexual Offences)
The POCSO Act, enacted in 2012 by the Ministry of Women and Child Development, indeed sought to address the severe issue of child sexual abuse with more specific and stringent legal provisions.
Here are the key points:
- Child-Friendly System: The Act aimed to establish a legal framework conducive to trials that are sensitive and considerate of the child's well-being.
- Definition of Child: Any person below eighteen years of age was defined as a child under this Act.
- Preventing Re-Victimization: Measures were implemented to prevent the re-victimization of children within the judicial system.
- Different Forms of Child Abuse: The Act defined various forms of child abuse, including penetrative and non-penetrative assault, aggravated sexual assault (such as abuse by a person in a position of trust or authority), especially when the abused child is mentally ill.
- Mandatory Reporting: It made reporting such cases a legal duty. Failure to report such instances could lead to imprisonment or a fine.
- Timely Evidence Recording: The Act required the recording of a child's evidence within thirty days.
- Trial Period: The Special Court handling the matter was expected to complete the trial within a year from the date of acknowledging the abuse.
- Privacy and Support: Special provisions were made for the trial to be conducted in camera, with the presence of parents or a trusted individual during the proceedings.
- Punishment for Trafficking: Individuals involved in trafficking children for sexual purposes were also subject to punishment under this act.
Following severe cases of child rape, the Criminal Law Amendment Ordinance of 2018 was introduced.
Its notable features included:
- Increased Minimum Punishments: The minimum punishment for rape was raised to 10 years, and it was increased to 20 years for offenses against girls aged below 16 years.
- Stringent Punishment for Younger Victims: For rape committed against girls aged below 12 years, the minimum punishment was 20 years of rigorous imprisonment, with the possibility of life imprisonment or the death penalty.
- Accountability for Law Enforcement: Police officers committing rape were liable for a minimum of 10 years' rigorous imprisonment.
- Accelerated Processes: Investigation of rape cases was to be completed within two months, and appeals in rape cases were to be disposed of within six months.
- Restriction on Bail: No anticipatory bail could be granted to a person accused of raping a girl below 16 years of age.
These measures reflected a concerted effort to strengthen laws, ensure swifter justice, and provide enhanced protection for minors against sexual offenses.
School Health Service
School health is an important branch of community health. School health service is an economical and powerful means of raising community health, and more important in future generations.
Objectives of school health services:
- the promotion of positive health
- the prevention of disease
- Early diagnosis, treatment and follow up of defects
- Awakening health consciousness in children
- Provision of healthful environment
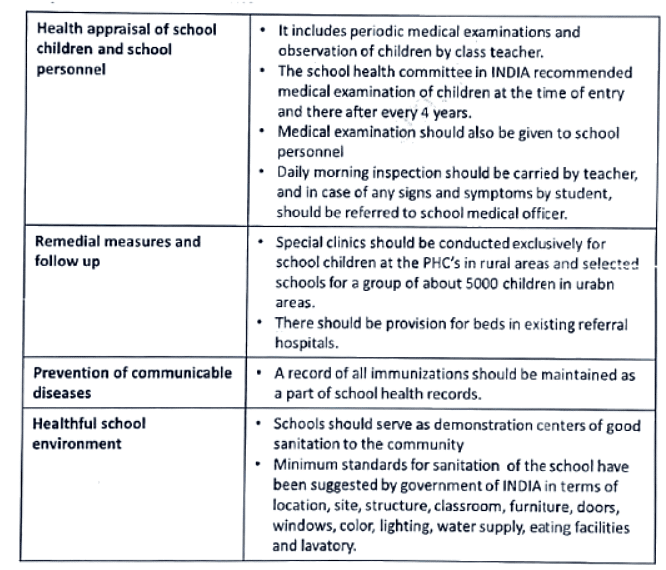
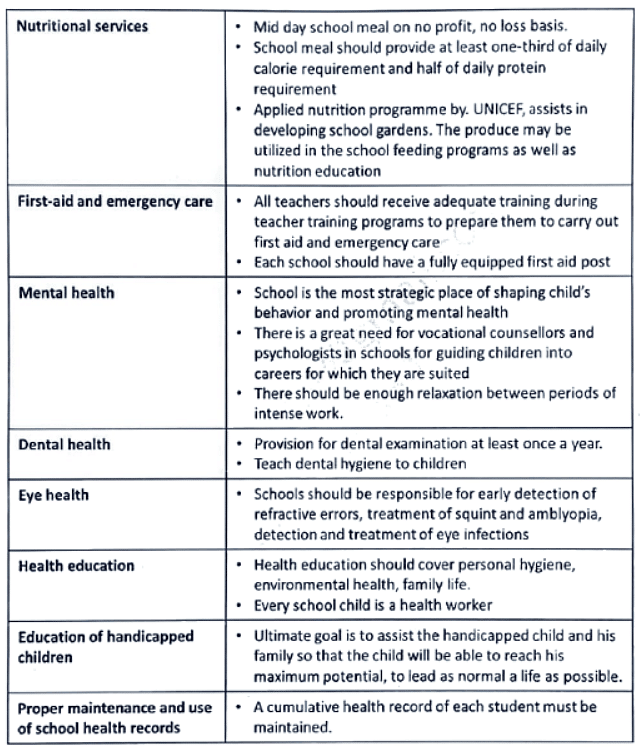
Aspects of school health service
NRHM-Repeats
Q1: Write briefly about key strategies of Natural Rural Health Mission. Describe the roles and responsibilities of an Accredited Social Health Activist. (2011)
Q2: Which of the existing Programmes of Health and Family Welfare have been integrated into the National Rural Health Mission? Underthe National Rural Health Mission (NRHM), what are the changes being carried out in the rural healthcare infrastructure in order to strengthen it? (2017)
Q3: What are the major responsibilities of ASHA in delivery of HBNC (Home based New Born Care-HBNC)? What is the specified schedule under which ASHA is expected to visit the newborn in a case of home delivery? (2019)
RMNCH-A Repeats
Q1: What are the primary objectives of Janani Suraksha Yojana? What are the salient features of this scheme? What is the ‘Vande Mataram Scheme’? How is it related to the Janani Suraksha Yojana? Enumerate various goals and targets set for Child Health in India. (2016)
Q2: Briefly discuss the proposed goals and targets under the Integrated Reproductive, Maternal, Newborn, Child and Adolescent Health in India (2015).
Q3: What is the objective of Pre conception Pre natal Diagnostic techniques (PCPNDT) Act? Enumerate the forms that must be filled by the attending doctors while carrying out a prenatal ultrasound. If a medical doctor is found to be violating the PCPNDT Act, what is the legal provision for punishment prescribed underthe Act? (2015)
Q4: Define "Infant Mortality Rate". List the major causes of IMR in India. What are the key steps that can bring down the IMR in lndia?(2015)
Q5: A high maternal mortality rate continues to be a major public health challenge before the country. Keeping that in context, answer the following questions:
i. How is "Maternal Mortality Rate" (MMR) defined?
ii. State the major causes of maternal mortality in the country.
iii. The recent data indicates a major decline in MMR in the country Briefly state, with due reasons, the various governmental initiatives which have led to this favorable decline in maternal mortality rate in India.
iv. The government has grouped the different states in the country in a specific manner to obtain a greater understanding of the ground situation and to map the changes following its initiatives. Briefly outline this strategy, and its benefits. (2018)
Q6: What do you understand by the term "Antenatal Pediatrics"? What are the various measures that can be undertaken to accomplish its primary objectives? (2019)
|
7 videos|219 docs
|
FAQs on NRHM & RMNCH-A: Preventive medicine in Obstetrics and Pediatrics - Medical Science Optional Notes for UPSC
| 1. What is the National Health Mission (NHM) and when was it established? |  |
| 2. What are the key strategies of the National Health Mission (NHM)? |  |
| 3. What are the initiatives undertaken by the NHM? |  |
| 4. What is the Menstrual Hygiene Scheme under NHM? |  |
| 5. How does NHM contribute to preventive medicine in obstetrics and pediatrics? |  |