Excretion | Animal Husbandry & Veterinary Science Optional for UPSC PDF Download
Kidney Structure Simplified
- Types of Nephrons:
- Mammalian kidneys have two types of nephrons.
- Distinguished by the location of glomeruli in the cortex and the extent of loops of Henle into the medulla.
- Cortical or Corticomedullary Nephrons:
- Glomeruli are in the peripheral cortex.
- Loops of Henle extend into the corticomedullary junction but rarely reach the outer medulla.
- Juxtamedullary Nephrons:
- Glomeruli are in the deeper cortex, near the corticomedullary junction.
- Loops of Henle, especially thin segments, extend deep into the medulla.
- Longer-looped nephrons may reach the medullary crest or renal papilla.
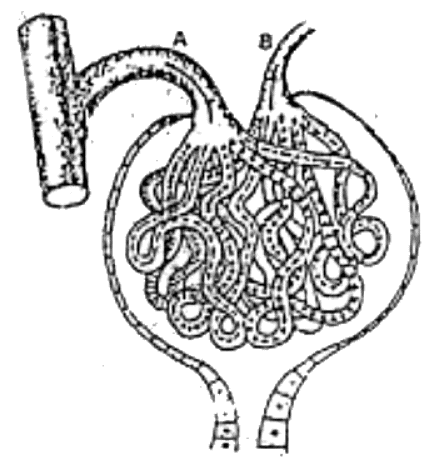
Fig. 12: Glomerulus showing the arrangement of twisted capillary loops and the absence of anastomoses. Note that the afferent vessel (A) is larger than the efferent vessel (B). The change in vessel size emphasizes the passage of fluid from the capillary bad to the expanded portion of the proximal convoluted tubule.
Kidney Structure Breakdown
Glomerulus Composition
- Capillary tuft between two arterioles.
- Tubular epithelium (Bowman's membrane) invaginated and surrounds glomerular capillaries.
- Basement membrane separates capillary endothelium from tubular epithelial cells.
- Podocytes (foot processes) on Bowman's membrane become less distinct in certain diseases.
Proximal Convoluted Tubule Cells
- Cuboidal or irregularly columnar cells.
- Rest upon a continuous basement membrane, separating tubular cells from peritubular capillary endothelium.
- Characterized by a brush border on the luminal surface.
- Microvilli on the luminal surface increase the surface area for reabsorptive functions.
- Abundant mitochondria and granular endoplasmic reticulum in the cytoplasm.
Henle's Loop Structure
- Composed of two segments with distinct cell types.
- Descending limb: Microvilli on luminal surfaces, complex structure, and interdigitations with adjacent cells.
- As it progresses into the medulla, cells become thinner, lose interdigitations.
- In the inner medulla, Henle's loops are difficult to differentiate between descending and ascending portions.
Henle's Loop and Tubules in the Kidney
- Thick Ascending Portion of Henle's Loop:
- Cells are cuboidal or columnar.
- Luminal border has short microvilli.
- Basal surface projections extend into the cytoplasm.
- Densely packed, elongated mitochondria are prominent.
- First Portion of Distal Convoluted Tubule:
- Similar to thick ascending segment of Henle's loop.
- Many mitochondria and densely packed ribonucleoprotein particles.
- Towards the collecting duct, fewer mitochondria and ribonucleoprotein particles, less prominent basal membrane projections.
- Collecting Duct Cells:
- Two cell types: light cells and intercalated (dark) cells.
- Light cells have light-staining cytoplasm, few organelles, and fewer ribosomes.
- Intercalated cells have more mitochondria and ribosomes.
- Postglomerular Blood Supply:
- Efferent arteriole divides into two types of vessels.
- One forms a dense capillary network around proximal and distal convoluted tubules in the cortex.
- Another group (vasa recta) enters the medulla, closely following thin segments of Henle's loops and collecting ducts.
- Vasa recta gives rise to capillary plexuses at different levels in the kidney.
- Vasa Recta in the Medulla:
- Form hairpin-like loops characteristic of thin segments of Henle's loop.
- Descending limbs of vasa recta form a capillary plexus, from which ascending limbs originate.
- Progressive decrease in descending capillary branches from cortex to medulla, resulting in a decrease in medullary blood flow.
- Interstitial Cells in the Kidney Medulla:
- Three distinctive types.
- First type found throughout the medullary substance, possibly producing specific prostaglandins.
- Second type considered collagen-forming cells.
- Third type shows properties suggestive of contractile activity.
Juxtaglomerular Complex
- Specialized cells in the wall of the afferent glomerular arterioles.
- Intimate contact with a distinctive part of the distal convoluted tubule called the macula densa.
- Cells in arteriolar walls termed granular or agranular based on the presence of secretory granules.
- Both cell types show active protein formation, with ribosomes and endoplasmic reticulum.
- Macula densa cells have specific staining characteristics and fewer mitochondria than other distal tubule cells.
Functions of Kidneys
- Conservation:
- Preserving water, fixed cations, glucose, and amino acids as needed by the body.
- Excess amounts excreted in urine.
- Elimination:
- Removing nitrogenous end products of protein metabolism (urea, creatinine, and ammonia).
- Excreting excess hydrogen ions for pH maintenance.
- Elimination of Organic Compounds:
- Disposing of complex organic compounds, both endogenous and exogenous.
- Endocrine Functions:
- Secretion of erythropoietin for normal hematopoiesis.
- Release of renin, involved in regulating aldosterone secretion by the adrenal cortex.
Renal Integration and Control
- Central nervous system (CNS) influences renal function through various pathways.
- Antidiuretic hormone (ADH) from the hypothalamo-neurohypophyseal complex aids in maximum urine concentration.
- Reflexes from peripheral receptors may affect renal function through CNS integration.
Regulation by Hormones
- Thyroid hormones and adrenohypophyseal growth hormone have trophic effects on the kidney.
- Major regulatory hormones are adrenal cortex steroids (cortisol type and aldosterone) and parathyroid hormone.
- Cortisol type steroids permit maximal water excretion, while aldosterone regulates potassium transport and sodium retention.
- Parathyroid hormone influences calcium and phosphate excretion into urine.
Kidney Structure Variation
- Most domestic animals' kidneys lack renal papillae; cow and man kidneys have papillae.
- Renal pyramids in cows and humans terminate in papillae, while others form medullary crests.
Urine Formation
- Starts as an ultrafiltrate of plasma, passing across glomerular capillary walls into Bowman's capsules and nephrons.
- Filtration process driven by blood pressure in glomerular capillaries and opposed by Colloid Osmotic Pressure (COP) of plasma proteins and intrinsic kidney tissue pressure.
Net Filtration Pressure
- Represents the pressure across the glomerulus in the kidneys.
- Determined by capillary blood pressure, colloid osmotic pressure (COP) of plasma proteins, and tissue pressure.
- Under normal conditions (arterial pressure of 90-100 mm Hg), net filtration pressure is around 45 mm Hg.
- Filtration ceases if blood pressure drops below a critical level (e.g., 45 mm Hg).
Intrarenal Blood Flow Distribution
- Approximately 85% of effective renal blood flow perfuses the cortex.
- Total renal blood flow is 42 ml/100 g/min, representing about 20% of cardiac output.
- Cortical flow: 472 ml/100 g/min, Outer medulla: 132 ml/100 g/min, Inner medulla: 17 ml/100 g/min, Hilar and perirenal fat: 21 ml/100 g/min.
Auto-regulation
- Kidney function is autonomous and highly developed in auto-regulation.
- Maintains relatively stable blood flow despite significant changes in arterial blood pressure.
Methods of Studying Nephron Function
- Nephron is the fundamental unit of a functional kidney.
- Micropuncture technique involves inserting micropipettes into nephrons to analyze small quantities of tubular fluid.
- Microelectrodes measure transcellular and transmembrane electrical potentials in different nephron segments.
Functions of Renal Tubules
- Glomeruli act primarily as filters.
- The glomerular membrane permits the passage of aqueous, ionic, and crystalloid components into Bowman's space.
- Erythrocytes and most plasma proteins do not filter through the glomerular membrane.
- Glomerular filtrate is an ultrafiltrate of plasma with minimal protein, mainly albumin.
- The filtrate composition is nearly identical to plasma before entering the proximal convolutions.
Proximal Tubule Function
- Micropipettes near the end of the proximal convoluted tubules collect fluid.
- Despite a 1:1 plasma cemolal ratio, changes in composition are observed.
- The proximal tubule cells return about 80% of glomerular filtrate to the blood.
- Glucose, amino acids, and most filtered protein are absent in this fluid.
Henle's Loop and Distal Tubule
- Tubular fluid passes through Henle's loop, becoming hypertonic in the medulla.
- Descending limb is permeable to long and crystalloids, adding sodium chloride and urea.
- Enters the distal convoluted tubule as a hypoosmotic fluid compared to plasma.
- Distal convoluted tubules receive hypotonic fluid from the medulla, representing 5% of original glomerular filtrate.
Collecting Ducts and Urine Concentration
- Collecting ducts carry urine to the renal pelvis, where final concentration occurs.
- In the presence of ADH, collecting ducts become permeable to water and urea.
- Water moves into the hypertonic medullary interstitium, increasing urea concentration.
- Resulting urine can be 5-7 times more concentrated than plasma.
Measurement of Renal Function
- Simplest method: Measure 24-hour urine output and relate it to water ingested.
- Doesn't provide details on filtration rate, total kidney blood flow, and relationships between filtration, solute excretion, and water reabsorption.
- Renal clearance concept used for more discrete aspects of renal function analysis.
Estimating Glomerular Filtration Rate (GFR)
- GFR estimation involves substances excreted in urine solely through glomerular filtration.
- If a stable concentration of the chemical in the blood is maintained, the urine flow rate reflects the excretion rate.
- Formula:
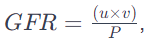 where u is urine concentration, v is urine flow rate, and P is plasma concentration.
where u is urine concentration, v is urine flow rate, and P is plasma concentration. - Example: For a dog with a weight of 20 kg, urine flow of 4 ml/min, plasma concentration of 0.2 mg/ml, and urine concentration of 2.5 mg/ml, GFR is calculated as 56 ml/min.
- The GFR is the amount of plasma cleared of the substance per minute.
Clearance of the Chemical (C)
- Clearance measures the rate of glomerular filtration (CGFR).
- In the example, 56 ml of plasma are cleared of the chemical X every minute.
- Various compounds like inulin and creatinine are used for GFR estimation.
- Creatinine clearance is a reasonable indicator of GFR in dogs.
Renal Clearance Techniques
- Used to estimate effective renal plasma flow, the amount of plasma perfusing functioning renal tissue.
- Certain substances are filtered and actively transported into tubular fluid, allowing measurement of renal plasma flow.
- Para-amino hippurate (PAH) is commonly used to estimate effective renal plasma flow.
Renal Clearance and Filtration
- Renal clearance shows how a substance is excreted in urine.
- Ratio of individual clearances (e.g., PAH and creatinine) indicates the degree of renal excretion through filtration and tubular function.
- Urea clearance is used as an indirect measure of Glomerular Filtration Rate (GFR).
Renal Regulation of Acid-Base Balance
- Normal conditions involve a continuous addition of acids or bases to body fluids.
- Maintaining a constant hydrogen ion concentration is crucial for balance.
- Acidosis occurs when blood pH drops, and alkalemia occurs when it rises.
- Mechanisms to combat disturbances include chemical buffering, respiratory adjustment, and renal excretion of hydrogen ions or bicarbonate.
Mechanisms to Combat Disturbances
- Chemical Buffering: Rapid response within minutes to prevent significant shifts in hydrogen ion concentration.
- Respiratory Adjustment: Alters blood carbonic acid concentration in response to disturbances like insufficient ventilation.
- Renal Excretion: Kidneys regulate acid-base balance through excretion of hydrogen ions or bicarbonate.
Metabolic Processes
Metabolism of organic compounds results in the formation of water, carbon dioxide, and urea within the body.
Elimination of Metabolic Byproducts
- Carbon Dioxide (CO2):
- Volatile nature leads to expiration through the respiratory system.
- Sulphur-Containing Amino Acids:
- Yield non-volatile sulphuric acid.
- Interacts with basic salts, buffered, and regulated by the kidneys.
Compounds and Acid-Base Balance
- Ammonium Chloride:
- Acidic, produces hydrogen ions and ammonia.
- Ammonia used for urea synthesis, and hydrogen ions contribute to acidemia.
- Kidneys excrete excess hydrogen ions to restore balance.
- Potassium Citrate (from plant-based foods):
- Metabolized to CO2 and water.
- Hydrogen ions produced contribute to alkalinity.
- Alkaline urine results, containing potassium and other cations.
Dietary Influence on Urine pH
- Acidic Urine: Common in carnivores, omnivores on high-protein diets, and fasting animals.
- Alkaline Urine: Seen in herbivores like ruminants and equines.
Physiological Constituents of Urine
- Composition:
- Nitrogen and sulphur metabolism byproducts, inorganic salts, and pigments.
- Typically yellowish in color.
- Consistency and Odor:
- Usually watery, but can be thick in horses due to mucous gland secretion.
- Characteristic odor varies among species.
- Specific Gravity (Average and Range):
- Cat: 1.030 (1.020 - 1.040)
- Cattle: 1.032 (1.030 - 1.045)
- Dog: 1.025 (1.016 - 1.060)
- Goat: 1.030 (1.015 - 1.045)
- Horse: 1.040 (1.025 - 1.060)
- Sheep: 1.030 (1.015 - 1.045)
- Swine: 1.012 (1.010 - 1.050)
- Man: 1.020 (1.002 - 1.040)
Note: Specific gravity indicates urine concentration, with higher values indicating more concentrated urine.
Amount of Urine
- Daily urine output varies based on factors like food, work, temperature, water intake, and season.
- Pathological variations can also affect urine amount.
Renal Insufficiency and Failure
- Renal efficiency relies on nephron function.
- Insufficiency can result from issues in renal blood flow, glomerular filtration rate, and tubular reabsorption.
- Vasomotor control affects renal blood flow, but diseases impacting it are usually linked to emergencies like shock or dehydration.
- Tubular necrosis may follow prolonged renal ischemia, causing renal insufficiency.
Glomerular Filtration and Tubular Reabsorption
- Disease states may affect glomerular filtration and tubular reabsorption independently.
- In conditions like hemoglobinuric nephrosis, glomerular filtration remains unaffected, but tubular reabsorption is significantly reduced.
- Damage to any part of the nephron tends to affect other parts due to the common blood supply.
Progression of Renal Disease
- Glomerulonephritis primarily affects glomeruli, but secondary tubular involvement occurs.
- In nephrosis, the primary lesion is in the tubules, and interstitial nephritis may lead to tubular degeneration followed by glomerular dysfunction.
Renal Dysfunction and Failure
- The development of renal dysfunction depends on the loss of functional renal tissue.
- Renal failure occurs when the degree of loss is so significant that the animal cannot continue to exist.
- Uremia, a clinical syndrome, manifests in cases of renal failure.
Pathological Physiology of Renal Insufficiency
- Damage to glomerular epithelium allows plasma proteins, mainly albumin, to pass into the capsular fluid.
- Anuria (complete cessation of glomerular filtration) may occur in severe cases.
- Compensatory response in less severe damage involves increased filtration per nephron, but tubular damage may lead to an inability to concentrate urine, characteristic of developing renal insufficiency.
Effects of Loss of Glomerular Filtration
- Loss of glomerular filtration results in the retention of urea and other nitrogenous end-products in the blood.
- Blood urea levels, though not significant for clinical signs, are used to measure glomerular filtration rate.
- In horses, renal tubular dysfunction can lead to bicarbonate loss and hyperchloremia.
Complications of Tubular Reabsorptive Function Loss
- Tubular reabsorptive function loss leads to continued sodium loss, causing hyponatremia in nephritis cases.
- Loss of large fluid quantities in poorly concentrated urine may cause clinical dehydration.
- Patients become susceptible to further fluid loss, shock, or circulatory emergencies.
Pathogenesis of Renal Failure
- Terminal stage (renal failure) results from disturbed renal excretory and homeostatic functions.
- Continued excretion of large volumes of dilute urine causes dehydration.
- Acute renal ischemia follows, leading to acute renal failure.
- Hypoproteinemia, acidosis, hyponatremia, hyperkalemia, and hypercalcemia contribute to clinical signs.
Manifestations and Causes of Renal Failure
- Renal failure is manifested by uremia, characterized biochemically by increased blood levels of total and urea nitrogen.
- Prerenal causes include congestive heart failure, acute circulatory failure, hemoglobinuric, and myoglobinuric nephrosis.
- Renal causes encompass glomerulonephritis, interstitial nephritis, pyelonephritis, embolic nephritis, and amyloidosis.
- Uremia may occur due to postrenal causes, such as complete urinary tract obstruction by calculi or internal rupture.
Experimental Induction and Variations
- Experimental induction of renal failure in ponies using substances like mercuric chloride has been done.
- Uremia can also result from surgical removal of both kidneys, showing different results than naturally occurring renal failure.
Causes of Uremia
- Uremia can result from prerenal, renal, or postrenal causes.
- Prerenal causes involve circulatory issues, while renal causes include various types of nephritis.
- Postrenal causes involve complete urinary tract obstruction by calculi or internal ruptures in the urinary tract.
Passive Venous Congestion
- Definition: Congestion is a condition where there's an increased amount of blood in the body's blood vessels.
Types of Congestion
- Passive Congestion: Decreased blood outflow from an organ, causing blood accumulation in the venous side of blood vessels.
Acute vs. Chronic Passive Congestion
- Acute Local Passive Congestion:
- Causes: Sudden blockage or pressure on veins.
- Examples: Strangulated hernia, Volvulus, Intussusception.
- Effect: Thin-walled veins are compressed, leading to blood accumulation in the area.
- Result: Increased tissue tension, diminished arterial flow, oxygen and nutrition shortage, potential necrosis, and later, gangrene.
- Acute General Passive Congestion:
- Main Cause: Acute heart failure resulting in diminished blood pressure.
- Occurrence: Before death, during asphyxia, or in cases of shock.
- Macroscopic Signs: Swollen, bluish-red (cyanotic) appearance due to the presence of a large amount of venous blood.
- Microscopic Signs: Veins and capillaries filled with blood; if liver and spleen are affected, sinusoids are engorged.
Chronic Passive Congestion
Local vs. General:
- Local: Limited to a specific area.
- General: Affects the entire body.
Note: Passive congestion can have severe consequences, including compromised blood flow, oxygen deprivation, tissue damage, and, in chronic cases, long-term organ dysfunction.
Chronic Local Passive Congestion
Causes
- Obstruction from Within:
- Often caused by blood clot formation (thrombosis).
- Pressure from Outside:
- Due to expanding tumors.
- Enlarged lymph nodes or their absence.
- Tight bandages on legs.
- Contracting scar tissue.
- Conditions like hydrocele, as seen in varicose veins of legs.
Macroscopic Signs
- Organs initially enlarge; later, fibrosis makes them smaller.
- Bluish-cyanotic appearance due to unoxygenated blood.
Microscopic Signs
- Venules and capillaries show engorgement.
- Edematous fluid separates cells and fibers.
- Cells may atrophy, and increased fibrous tissue is evident.
Chronic General Passive Congestion
Causes
- Heart Lesions:
- Stenosis of valvular openings.
- Valvular insufficiency.
- Chronic myocardial failure.
- Constrictive pericarditis.
- Pulmonary Lesions:
- Emphysema.
- Chronic interstitial pneumonia.
General Changes
- Decreased Circulation Leads to:
- Hypoxia (oxygen shortage).
- Decreased nutrition.
- Accumulation of waste products.
- Increased vascular permeability (damage to endothelium).
- Sodium retention: Kidney, liver, and adrenal damage affect sodium excretion; reabsorption leads to increased blood volume and venous pressure.
- Resulting Effects:
- Cell atrophy and regression followed by fibrosis.
- Hemorrhage occurs.
- Edema develops.
Summary: Chronic venous congestion results in various changes like decreased circulation, hypoxia, reduced nutrition, waste accumulation, increased permeability, sodium retention, cell atrophy, fibrosis, hemorrhage, and edema. These changes are seen in both local and general cases.
Sweat Glands in Elephants
Elephants do not have sweat glands.
Thermoregulatory Sweating
- Sweating helps regulate body temperature.
- It occurs when warm blood stimulates the hypothalamic thermoregulatory center.
- Afferent nerve impulses from the periphery also stimulate the thermoregulatory center.
Sweat Composition
- Sweat is considered similar to urine but is the most dilute animal fluid.
- It has small quantities of solid constituents, making it unlikely to play a significant role in excretion.
Biochemical Tests for Urinary Dysfunction
- Urine examination is a key test for diagnosing diseases related to the urinary system.
- Kidneys play a crucial role in water, acid-base, and electrolyte balance, reflecting in urine quality.
- Physical qualities like color, transparency, odor, specific gravity, and pH are examined.
- Biochemical tests include checking for albumin, glucose, ketone bodies, blood, and bile pigment.
- Microscopic examination assesses the urinary sediment.
Albumin Presence
Presence of albumin (proteinuria) in nephritis, acute interstitial nephritis, chronic interstitial nephritis, pyelonephritis, nephrosis, renal congestion, amyloidosis, renal infarction, and neoplasms.
Haematuria and Haemoglobinuria
- Haematuria (whole blood in urine) indicates kidney or urinary tract issues.
- Haemoglobinuria indicates kidney or urinary tract problems or certain protozoan diseases.
Microscopic Examination
Presence of epithelial cells, erythrocytes, leucocytes, casts, mucous threads, parasite eggs, bacteria, or crystals indicates various urinary tract conditions.
Diseases of Other Organs
Presence of glucose, ketone bodies, bile pigment, and fat can indicate diabetes mellitus, acetonemia, liver conditions, obesity, hypothyroidism, or diabetes mellitus.
FAQs on Excretion - Animal Husbandry & Veterinary Science Optional for UPSC
| 1. What is the structure of the kidney? |  |
| 2. What is the role of Henle's loop and tubules in the kidney? |  |
| 3. What are the functions of the kidneys? |  |
| 4. What are metabolic processes in the kidneys? |  |
| 5. What is chronic general passive congestion of the kidneys? |  |















