Embryology - 3 Chapter Notes | Anatomy - NEET PG PDF Download
Renal System
The genitourinary system primarily originates from the intermediate mesoderm, with contributions from the endoderm of the hindgut for the distal parts of the tubes.
- The intermediate mesoderm gives rise to the urogenital ridge, a raised area along the body’s back wall.
- Part of this ridge develops into the nephrogenic cord, which is crucial for forming the urinary system.
- The nephrogenic cord eventually leads to the development of three kidney structures:
(a) Pronephros
- The pronephros forms from the differentiation of mesoderm in the nephrogenic cord, creating pronephric tubules and a duct.
- It is the uppermost kidney structure, developing in the neck region.
- The pronephros is temporary and regresses completely by the fourth week of development.
(b) Mesonephros
- The mesonephros forms from the differentiation of mesoderm in the nephrogenic cord, producing mesonephric tubules and the mesonephric duct, also known as the Wolffian duct.
- This structure develops in the chest and lower back areas and is partially temporary.
- Most mesonephric tubules regress, but the mesonephric duct remains, connecting to the urogenital sinus.
- In males, the mesonephric duct forms a pathway for sperm from the testes to the urethra. In females, the Wolffian duct regresses, leaving non-functional remnants.
(c) Metanephros
- The metanephros develops from a growth of the mesonephric duct called the ureteric bud and a condensation of mesoderm in the nephrogenic cord known as the metanephric mesoderm.
- This structure is the lowest kidney formation, beginning around the fifth week and becoming functional by the tenth week of development.
- Unlike the smooth adult kidney, the fetal kidney has lobes.
The metanephros eventually becomes the permanent kidney, comprising the excretory system and the collecting system.
- The excretory system consists of nephrons, while the collecting system originates from the ureteric bud, an outgrowth of the mesonephric duct.
- The ureteric bud is responsible for forming the ureter, renal pelvis, major and minor calyces, and the entire collecting system.
- Proper connection between the collecting system and the excretory tubules is essential for normal kidney development.
Ascent of the Kidneys
- Initially, the fetal metanephros is located at the vertebral levels S1–S2, while the adult kidney is situated at T12–L3.
- The change in position occurs because the lower part of the embryo grows more than the metanephros.
- During this ascent, the kidneys rotate 90°, causing the hilum, which initially faces downward, to turn inward.
- Blood vessels from the kidneys grow towards and invade the common iliac arteries while the kidneys are still in the pelvis.
- As the embryo lengthens, the kidneys ascend to their final position in the lower back area.
- Instead of bringing their blood supply with them, the kidneys develop new branches higher up and allow the lower ones to regress.
- Eventually, the renal arteries branch off from the abdominal aorta.
- Some arteries formed during this ascent may persist as supernumerary arteries, which are end arteries. Damage to these arteries can lead to kidney tissue death.
Development of the Collecting System
- The ureteric bud, an outgrowth of the mesonephric duct, penetrates the metanephric mesoderm and undergoes repeated branching.
- This branching forms the ureter, renal pelvis, major calyces, minor calyces, and collecting ducts.
Development of the Nephron
- The collecting ducts exert an inductive influence on the metanephric mesoderm, causing it to differentiate into metanephric vesicles.
- These vesicles develop into primitive S-shaped renal tubules, which are essential for nephron formation.
- The renal tubules further differentiate into the connecting tubule, distal convoluted tubule, loop of Henle, proximal convoluted tubule, and Bowman’s capsule.
- Glomeruli, tufts of capillaries, protrude into Bowman’s capsule.
- Nephron formation is complete at birth, but functional maturation continues throughout infancy.
Embryonic Origins and Adult Derivatives:
- Metanephric Mesoderm:
- Forms metanephric vesicles and S-shaped renal tubules, which give rise to:
- Connecting tubule
- Distal convoluted tubule
- Loop of Henle
- Proximal convoluted tubule
- Renal (Bowman’s) capsule
- Renal glomerulus
- Forms metanephric vesicles and S-shaped renal tubules, which give rise to:
- Ureteric Bud:
- Develops into:
- Ureter
- Renal pelvis
- Major calyx
- Minor calyx
- Collecting duct
- Develops into:
Urinary Bladder and Urethra
The urinary bladder develops from the upper part of the urogenital sinus, which is connected to the allantois.
- In adults, the allantois becomes a fibrous cord known as the urachus or median umbilical ligament.
- The trigone of the bladder is formed when the lower ends of the mesonephric ducts merge into the back wall of the bladder.
The allantois is an outgrowth from the endoderm that extends from the front part of the urogenital sinus to the umbilicus.
- Eventually, its far end, called the urachus, changes into a fibrous cord that becomes the median umbilical ligament.
- If the urachus remains open, it can result in a urachal fistula or cyst in that region.
Development of the Urinary Bladder
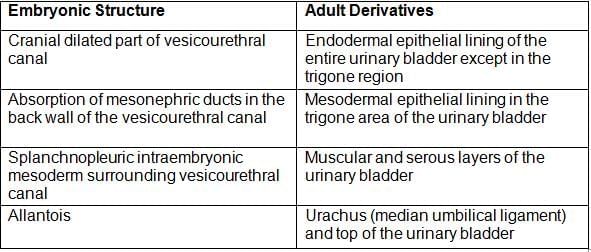
- In both sexes, the mesonephric (Wolffian) duct produces a ureteric bud on each side, which develops into the ureter, the pelvic region of the ureter, the major and minor calyces, and the kidney's collecting tubules.
- The lower end of the ureteric bud is absorbed into the developing bladder, contributing to the formation of the trigone and part of the urethra.
- The terminal portion of mesonephric duct is absorbed into the rear wall of the urinary bladder, leading to the formation of the trigone, which is made of mesodermal tissue.
Note:
- The upper part of the mesonephric duct (Wolffian duct) serves as a passage for sperm from the testes to the urethra and develops into the epididymis, ductus deferens, seminal vesicle, and common ejaculatory duct. In females, these ducts regress.
- Renal agenesis occurs when the ureteric bud does not develop, preventing the formation of metanephric vesicles and nephrons.
- Congenital polycystic kidney disease is caused by genetic factors resulting in abnormal kidney structure. The glomeruli continue to produce urine, which collects in the tubules due to lack of an outlet, causing the tubules to undergo cystic enlargements (retention cysts).
- Pelvic kidney is an ectopic kidney that remains in the pelvis when it fails to ascend. Two pelvic kidneys may merge to form a solid lobed organ called a cake (rosette) kidney.
- A horseshoe kidney results from the lower poles of both kidneys fusing during development. The ureters pass in front of the isthmus and may become obstructed due to pressure. The inferior mesenteric artery also passes in front of the isthmus, and the horseshoe kidney can become trapped behind it as it tries to move up to its normal adult position.
- Bladder exstrophy is a ventral body wall defect that occurs due to incomplete closure of the lateral body wall folds in the pelvic area, causing the bladder to protrude through the defect.
- Urachal fistula or cyst arises when a remnant of the allantois persists, forming a fistula or cyst along the midline from the umbilicus to the top of the urinary bladder. A urachal fistula creates a direct link between the urinary bladder and the outside body at the umbilicus, leading to urine draining from the umbilicus.
Genital System
- The genital system comprises the gonads (or primitive sex glands), genital ducts, and external genitalia.
- The determination of an individual's sex occurs around week 7 during the sexually indifferent stage of embryonic development.
- Sexually Indifferent Embryo: The embryo's genetic sex (46,XX for female or 46,XY for male) is established at fertilization. During the first six weeks, the embryo remains in a sexually indifferent state, appearing the same regardless of its genetic sex.
- It is only after week 7 that the embryo begins to show signs of sexual differentiation.
- By week 12, the external genitalia can be identified as either female or male. By week 20, the process of sexual differentiation is complete.
- Phenotypic sexual differentiation is guided by the SRY gene located on the Y chromosome, leading to the development of male, female, or intersex characteristics.
- The SRY gene produces a protein called testes-determining factor (TDF), which plays a crucial role in sexual differentiation.
- In the presence of the SRY gene:
- Medullary (testis) cords develop.
- The tunica albuginea forms.
- Cortical (ovarian) cords do not develop.
- In the absence of the SRY gene, ovarian development occurs, influenced by the gene WNT4. This leads to:
- The formation of ovaries with typical cortical cords.
- The disappearance of medullary (testis) cords.
- The failure of the tunica albuginea to form.
- Primordial germ cells originate from epiblast cells at the primitive streak, migrate to the endoderm of the yolk sac, and eventually reach the genital ridge between weeks 4 and 6 of development.
- During the indifferent stage, both the mesonephric duct and the paramesonephric duct systems are present.
- In males, testosterone produced by Leydig cells in the testes stimulates the development of the mesonephric ducts into various structures, including the efferent ducts, epididymis, vas deferens, seminal vesicle, and ejaculatory duct.
- Müllerian inhibiting substance (also known as anti-Müllerian hormone), produced by Sertoli cells in the testes, causes the regression of the paramesonephric (Müllerian) ducts.
- Dihydrotestosterone (DHT) further stimulates the development of male external genitalia, including the penis and scrotum.
- In the absence of testosterone, estrogens regulate the development of the paramesonephric ducts in females, leading to the formation of the uterus, uterine tubes, and the upper part of the vagina.
- Estrogens also promote the differentiation of female external genitalia, including the clitoris, labia, and the lower part of the vagina.
Embryonic structures and their homologous adult derivatives in male and female.
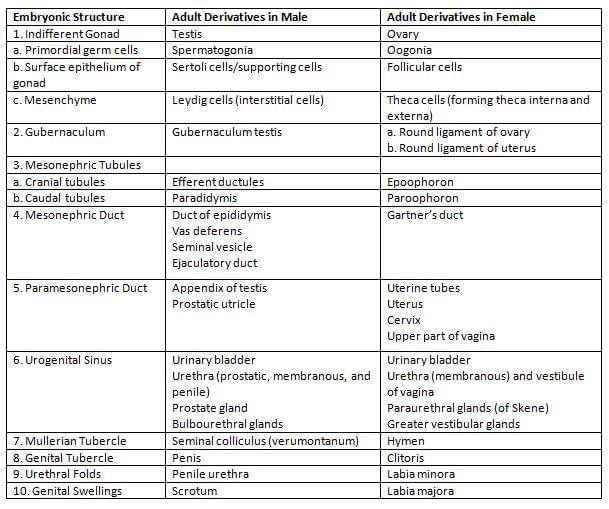
The urogenital sinus comprises three parts:
- the cephalad or vesicle portion, which develops into the urinary bladder;
- the middle or pelvic portion, which gives rise to the female urethra; and
- the caudal or phallic part, which forms the distal vagina and the greater vestibular (Bartholin) and paraurethral (Skene) glands.
- Gubernaculumis an embryonic structure composed of undifferentiated mesenchyme that connects to the caudal end of the gonads (testes and ovaries).
- As the scrotum and labia majora develop in males and females, respectively, the gubernaculum assists in the descent of the gonads.
- The testes descend further than the ovaries, passing through the inguinal canal.
Flowchart 3: Influence of chromosome complement of primordial germ cells on indifferent gonad.
Table 9: Differences in the development of testis and ovary.
- Testis:
- Only one generation of sex cords (medullary cords) is formed, which gives rise to seminiferous tubules and rete testis.
- Ovary:
- Multiple generations of sex cords are formed, leading to the development of ovarian follicles.
Male Reproductive System
Testis
- The testis develops from the intermediate mesoderm, forming a ridge known as the urogenital ridge, which later becomes the gonadal ridge.
- From the gonadal ridge, primary sex cords form and include primordial germ cells with an XY genotype, which migrate from the yolk sac.
- These cords differentiate into the medulla of the gonad and separate from the surface epithelium as the tunica albuginea thickens.
- Over time, primary sex cords transform into seminiferous cords, tubuli recti, and rete testes.
- Seminiferous cords are composed of primordial germ cells and Sertoli cells, which produce Mullerian Inhibiting Factor (MIF).
- The mesoderm between these cords gives rise to Leydig cells, responsible for secreting testosterone.
- Initially, seminiferous cords are solid, but at puberty, they develop a lumen and become seminiferous tubules.
Descent of Testis
- The testis begins its journey in the abdomen, moving down to the pelvis and eventually into the scrotum. This descent is facilitated by the uneven growth of the upper abdomen.
- The gubernaculum plays a crucial role by pulling the lower part of the testis down to the scrotum and securing it in place.
- Along with the gubernaculum, the peritoneum forms an invagination called the processus vaginalis. Most of this structure is later absorbed, leaving behind the distal end, which becomes the tunica vaginalis.
- The timeline for the descent of the testis is as follows:
- 2nd Month (7th Week). The testis is located in the abdomen.
- 3rd Month. The testis descends into the pelvis.
- 6th Month (End). The testis reaches the deep inguinal ring.
- 7th Month. The testis passes through the inguinal canal.
- 8th Month. The testis is at the superficial inguinal ring.
- 9th Month (Beginning). The testis enters the scrotum.
- 9th Month (End) or Shortly After Birth. The testis reaches its final position in the scrotum.
Development of the Genital Ducts
- In males, the mesonephric ducts develop as part of the urinary system and are also involved in forming the definitive metanephric kidney.
- These ducts give rise to various structures, including the epididymis, ductus deferens, seminal vesicle, and ejaculatory duct.
Figs. 64A to D: Descent of gonads from the abdominal region, pulled by gubernaculum.
Position of Testis
- Abdomen: 2nd month (7th week)
- Pelvis (Iliac fossa): During 3rd month (12th week)
- Deep inguinal ring: At the end of 6th month (24th week)
- Passing through inguinal canal: During 7th month (25–28 week)
- At superficial inguinal ring: Eighth month (29–32 week)
- Enters scrotum: Beginning of ninth month (33 week)
- At the base of scrotum: Before birth (End of 9th month/36th week)
Fig. 65: Two pairs of genital ducts during the indifferent stage of development of gonads.
- Some mesonephric tubules in the area of the testis develop into the efferent ductules.
- In adult males, remnants of the mesonephric duct (known as the appendix epididymis) and tubules (called the paradidymis) may be present.
Paramesonephric Ducts
- The upper parts of the paramesonephric ducts and the uterovaginal primordium regress under the influence of Mullerian Inhibiting Factor (MIF).
- In adult males, remnants of the paramesonephric duct, referred to as the appendix testis, may be found.
Female Reproductive System
Formation of Ovaries
- The ovary develops from the intermediate mesoderm, forming a structure along the back wall called the urogenital ridge, which later becomes the gonadal ridge.
- Primary sex cords originate from this gonadal ridge, containing primordial germ cells (XX genotype) that migrate from the yolk sac wall.
- These primary sex cords extend into the medulla and give rise to the rete ovarii, which eventually disappears.
- Secondary sex cords develop and include primordial germ cells as a thin layer called the tunica albuginea forms.
- These secondary sex cords separate to create clusters of cells known as primordial follicles, containing primary oocytes surrounded by simple squamous cells.
Development of Genital Ducts
Paramesonephric (Müllerian Ducts)
- The upper (unfused) parts of the paramesonephric ducts develop into the uterine tubes.
- The lower parts of the paramesonephric ducts join in the center to create the uterovaginal primordium, which develops into the uterus, cervix, and the upper third of the vagina.
- The paramesonephric ducts extend into the back wall of the cloaca, leading to the creation of the sinovaginal bulbs.
- The sinovaginal bulbs merge to form the solid vaginal plate, which develops into the lower two-thirds of the vagina.
- Vestigial remnants of the paramesonephric duct may be present in adult females, known as the hydatid of Morgagni.
Mesonephric (Wolffian Ducts and Tubules)
- In females, mesonephric ducts develop as part of the urinary system and are crucial for forming the definitive metanephric kidney, although they degenerate after this kidney is formed.
- Vestigial remnants of the mesonephric ducts may exist in adult females, known as the appendix vesiculosa and Gartner’s duct.
- Remnants of the mesonephric tubules are identified as the epoophoron and the paroophoron.
Development of the Vagina
- The upper third of the vagina arises from the Müllerian (paramesonephric) duct (mesoderm), while the lower two-thirds develop from the endoderm of the urogenital sinus.
- The lower sections of the Müllerian ducts fuse in the midline to form the uterovaginal primordium, contributing to the upper third of the vagina.
- The paramesonephric ducts extend into the back wall of the cloaca (urogenital sinus) and stimulate the formation of the sinovaginal bulbs.
- The sinovaginal bulbs merge to create the solid vaginal plate, which subsequently forms the lower two-thirds of the vagina.
- Human chorionic gonadotrophin (hCG) is a hormone produced by the syncytiotrophoblast. It supports the corpus luteum in producing progesterone to maintain its function.
- hCG can be detected in maternal blood from day 8 and in urine from day 10 using radioimmunoassay (RIA) methods targeting the β-subunit of hCG.
External Genitalia
Male External Genitalia
- The phallus develops into the penis, which includes the glans penis, corpora cavernosa penis, and corpus spongiosum penis.
- The urogenital folds form the ventral side of the penis, known as the penile raphe.
- The labioscrotal swellings mature into the scrotum.
Female External Genitalia
- The phallus becomes the clitoris, which consists of the glans clitoris, corpora cavernosa clitoris, and vestibular bulbs.
- The urogenital folds give rise to the labia minora.
- The labioscrotal swellings develop into the labia majora, while the mons pubis comes from a different embryological source.
- The clitoris originates from the genital tubercle.
- The labia majora are formed from the genital swellings.
- The external genitalia are derived from the somatopleuric lateral plate mesoderm.
Skeletal System
Vertebrae are formed from the paraxial mesoderm, which creates somites. A part of the somite called the sclerotome is responsible for the formation of vertebrae. Sclerotomes surround the notochord and extend to cover the neural tube, dividing into three sections:
- Ventral sclerotomes. These develop into the vertebral body and the annulus fibrosus.
- Lateral sclerotomes. These form the vertebral arch, including the pedicle and lamina.
- Dorsal sclerotomes. These are responsible for creating the spinous process.
Ribs develop from the costal processes of the sclerotome part of the somite, which becomes the costal processes of the thoracic vertebrae. Primary ossification centres appear in the rib body and mostly convert to cartilage during weeks 13–14 of development.
Endocrine System
Adrenal Gland Embryology
- The development of the cortex begins in the second month of pregnancy as part of the formation of the adrenal gland. It originates from the coelomic epithelium in the intermediate mesoderm.
- During this process, cells migrate into the underlying mesenchyme, which is situated between the base of the dorsal mesogastrium and the mesonephros.
- A mesenchymal capsule forms around the cortex from both the front and back, and this capsule is derived from the mesonephros.
- The medulla of the adrenal gland is composed of neural crest cells that differentiate into chromaffin cells.
Upper Limb and Lower Limb Development
- Limbs begin to develop at the end of the fourth week as buds along the body wall, guided by HOX genes which determine their position. The upper limb is associated with spinal segments C5–T2, while the lower limb is linked to L2–S2.
- The lower limb develops approximately 1 to 2 days later than the upper limb.
Upper Limb and Lower Limb Arteries
The development of arteries in the upper and lower limbs follows a specific pattern and timeline, as detailed below:
Upper Limb Arteries
- The axis artery of the upper limb originates from the seventh cervical intersegmental artery.
- This artery runs along the front of the lower limb and terminates in a palmar capillary plexus in the hand.
- The main trunk of the axis artery branches into the axillary artery, brachial artery, anterior interosseous artery, and deep palmar arch.
- The digital arteries of the hand stem from the palmar capillary plexus.
- The median artery forms from the anterior interosseous artery and connects to the palmar capillary plexus.
- The radial and ulnar arteries branch off the axis artery near the elbow bend.
- The fourth aortic arch contributes to the upper part of the right subclavian artery.
- The seventh intersegmental artery (ISA-7) aids in forming the axial artery of the upper limb and contributes to the lower part of the right subclavian artery and the entire left subclavian artery.
- The subclavian artery (both right and left) extends into the limb bud as the axis artery, ending in a terminal plexus near the tip of the limb bud.
- The axis artery persists in adults as the axillary artery, brachial artery, anterior interosseous artery, and deep palmar arch.
- During development, the radial artery is pre-axial, and the ulnar artery is post-axial.
Lower Limb Arteries
- The axis artery of the lower limb is derived from the fifth lumbar intersegmental artery.
- This artery runs along the back of the lower limb.
- It branches into the inferior gluteal artery, a small artery accompanying the sciatic nerve (sciatic artery), part of the popliteal artery (above the popliteus muscle), the lower section of the peroneal artery, and part of the plantar arch.
- The femoral artery is a newly formed vessel that appears on the front of the thigh.
- It connects with the external iliac artery above and the popliteal artery below.
- The external iliac artery branches from the axial artery.
|
42 docs|7 tests
|
FAQs on Embryology - 3 Chapter Notes - Anatomy - NEET PG
| 1. What is the developmental origin of the urinary bladder in human embryology? |  |
| 2. How do the male and female reproductive systems develop differently during embryogenesis? |  |
| 3. What are the main components of the skeletal system that develop during embryonic stages? |  |
| 4. What role does the endocrine system play in the development of the urinary and genital systems? |  |
| 5. How does limb development occur during embryogenesis? |  |
















