Neuroanatomy - 3 Chapter Notes | Anatomy - NEET PG PDF Download
Pons: Overview and Structure
The pons is a crucial part of the brainstem, situated between the midbrain above and the medulla oblongata below, and it lies in front of the cerebellum.
Structure of the Pons
The pons comprises two main sections: the basilar part at the front and the pontine tegmentum at the back.
Basilar Part: This section includes several important structures, such as:
- Corticobulbar Tracts: These tracts are involved in conveying signals from the cerebral cortex to the brainstem, playing a key role in motor control, especially for the face and neck.
- Corticospinal Tracts: These tracts transmit signals from the cortex to the spinal cord, facilitating voluntary motor control of the body.
- Corticopontine Tracts: These tracts send information from the cortex to the pons, which then relays it to the cerebellum for coordination of movement.
- Pontine Nuclei: These nuclei are involved in relaying signals from the cerebellum and are crucial for motor control and coordination.
Pontine Tegmentum:This part contains:
- Cranial Nerve Nuclei: These are clusters of neurons that serve as relay points for cranial nerves, which control various functions such as facial movement and sensation.
- Reticular Nuclei: These nuclei are part of the reticular formation, involved in regulating arousal, sleep, and attention.
- Major Ascending Sensory Pathways: These pathways carry sensory information from the body to the brain, playing a vital role in processing sensory input.
Cranial Nerves and Functions
- The pons houses the nuclei for several cranial nerves:
- Cranial Nerve V (Trigeminal Nerve): Responsible for sensation in the face and motor functions such as chewing.
- Cranial Nerve VI (Abducent Nerve): Controls the lateral movement of the eye.
- Cranial Nerve VII (Facial Nerve): Manages facial expressions, taste sensations from the anterior two-thirds of the tongue, and some glandular functions.
- The nuclei for the vestibulocochlear nerve, which is responsible for hearing and balance, are located at the junction of the pons and medulla.
- The pons also contains the center for lateral gaze, which coordinates horizontal eye movements.
- Additionally, the pons connects to the cerebellum through the middle cerebellar peduncle, facilitating communication between these two brain regions.
Transverse Section of the Pons
A cross-section of the pons reveals various structures, which can be categorized into medial and lateral components.
Medial Structures
- Medial Longitudinal Fasciculus:. bundle of nerve fibers involved in coordinating eye and head movements.
- Internal Genu of the Facial Nerve: Part of the facial nerve that contributes to the formation of the facial colliculus.
- Abducent Nucleus: Located beneath the facial colliculus, this nucleus controls the lateral rectus muscle, responsible for eye abduction.
- Medial Lemniscus:. pathway that transmits sensory information related to touch and proprioception to the brain.
- Corticospinal Tract: Situated at the base of the pons, this tract carries motor signals from the brain to the spinal cord.
Lateral Structures
- Facial Nucleus: Responsible for innervating the muscles of facial expression.
- Descending (Spinal) Sensory Nucleus and Tract of the Trigeminal Nerve: Involved in processing sensory information from the face.
- Lateral Spinothalamic Tract (Spinal Lemniscus): Transmits pain and temperature sensations to the thalamus.
- Vestibular and Cochlear Nuclei: Nuclei that process auditory and vestibular (balance) information.
Lower Part of the Pons
- Houses the nuclei of cranial nerves VI (Abducent), VII (Facial), and VIII (Vestibulocochlear).
- Contains the nucleus of the spinal tract of the trigeminal nerve, which is involved in pain and temperature sensation from the face.
Upper Part of the Pons
- Contains the motor and principal sensory nuclei of the trigeminal nerve, which are responsible for motor and sensory functions in the face.
- Includes the caudal part of the nucleus ceruleus, which is involved in the regulation of arousal and attention.
Medulla Oblongata
The medulla oblongata is situated at the lower part of the brainstem, where it connects to the spinal cord. The upper portion of the medulla joins with the pons. This structure extends from the inferior pontine sulcus to the pyramidal decussation.
Cranial Nerves
- The medulla contains the nuclei of cranial nerves IX to XII, which are the glossopharyngeal, vagus, cranial accessory, and hypoglossal nerves.
- Cranial Nerves IX and X are primarily involved in autonomic functions, while Cranial Nerves XI and XII focus on motor functions.
Functions of the Medulla
- The medulla is responsible for several vital centres, including those for:
- Cardiovascular regulation
- Respiratory function
- Vomiting
- Vasomotor control
- These centres play a crucial role in managing heart rate, breathing, and blood pressure.
Additionally, the medulla connects to the cerebellum through the inferior cerebellar peduncle.
Olive in the Medulla Oblongata
- The olive is a crucial part of the brain, made up of two oval structures located in the medulla oblongata. These structures contain the olivary nuclei.
- The olive is positioned on the front surface of the medulla, to the side of the pyramid. It is separated from the pyramid by the antero-lateral sulcus and the fibres of the hypoglossal nerve.
- At the back, the olive is separated from the posterolateral sulcus by the ventral spinocerebellar fasciculus. The space between the top of the olive and the pons contains the vestibulocochlear nerve.
- The superior olivary nucleus, located at the junction of the pons and medulla, plays a vital role in the auditory system and is an essential part of the pathway for hearing.
- The inferior olivary nucleus is involved in the olivo-cerebellar system and is primarily responsible for cerebellar motor learning and function.
Pyramid in the Medulla Oblongata
- The medulla oblongata features two paired, ridge-like structures known as medullary pyramids on its front side.
- These pyramids contain motor fibres from the pyramidal tracts, specifically the corticospinal and corticobulbar tracts.
- Pyramidal decussation occurs in the lower part of the medulla, where:
- About 90% of the fibres cross over to form the lateral corticospinal tract.
- The remaining 10% descend via the anterior corticospinal tract, crucial for voluntary motor control.
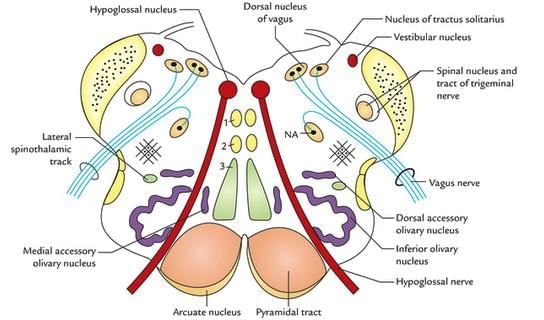
Structures Seen in a Transverse Section of the Medulla
Medial Structures:
- Hypoglossal Nucleus: Responsible for tongue movements.
- Medial Lemniscus: Carries sensory information about touch and proprioception.
- Pyramid: Contains corticospinal fibers involved in voluntary motor control.
Lateral Structures:
- Nucleus Ambiguus: Innervates muscles of the palate, pharynx, and larynx.
- Vestibular Nuclei: Involved in balance and spatial orientation.
- Inferior Cerebellar Peduncle: Connects the cerebellum to the medulla, carrying various tracts.
Tracts:
- Lateral Spinothalamic Tract: Carries pain and temperature sensations.
- Spinal Lemniscus:. sensory pathway for pain and temperature.
- Spinal Nucleus and Tract of Trigeminal Nerve: Involved in sensation from the face.
Medial Medullary Syndrome
- Caused by the occlusion of the vertebral artery, anterior spinal artery, or a branch of the basilar artery.
- Symptoms include:
- Flaccid paralysis and atrophy of one half of the tongue: Due to damage to the hypoglossal nerve (lower motor neuron injury).
- Spastic paralysis of the trunk and limbs: Resulting from involvement of the contralateral corticospinal tract (upper motor neuron injury).
- Impaired tactile, proprioceptive, and vibration sense: Affecting the trunk and limbs due to damage to the contralateral medial lemniscus.
Wallenberg Syndrome (Lateral Medullary Syndrome)
- Caused by the occlusion of the vertebral artery, often involving the posterior inferior cerebellar artery.
- Symptoms include:
- Loss of pain and temperature sensation on one side of the face: Due to involvement of the descending tract and nucleus of the trigeminal nerve.
- Cerebellar ataxia of the limbs: Characterized by uncoordinated movements and falling to the side of the lesion, possibly related to the spinocerebellar tract.
- Nystagmus, vertigo, and nausea: Resulting from involvement of the vestibular nucleus.
- Horner’s syndrome: Manifested as miosis (constricted pupil), ptosis (drooping eyelid), and anhidrosis (lack of sweating) due to damage to the descending sympathetic tract.
- Paralysis of palate, pharynx, and larynx muscles: Leading to difficulties in speech and swallowing, due to involvement of the nucleus ambiguus.
- Loss of taste on one half of the tongue: Due to damage to the nucleus tractus solitarius.
- Loss of pain and temperature sensation over half of the body: Due to involvement of the lateral spinothalamic tract.
Total Unilateral Medullary Syndrome
- Results from the occlusion of the vertebral artery.
- Presents with a combination of symptoms from both medial and lateral medullary syndromes.
Additional Points:
- Nucleus Fasciculatus: Also known as the cuneatus nucleus, is located in the medulla oblongata.
- Nuclei Cuneatus and Gracilis: Present in the medulla oblongata, involved in sensory processing.
- Facial Nerve: Does not arise from the medulla; it originates from the pons.
- Nucleus Ambiguus: Located postero-medial to the olive in the medulla.
- Olive:. structure seen in the medulla oblongata, involved in motor control.
- Internal Arcuate Fibres: These fibers come from the nucleus gracilis and cuneatus, cross to the opposite side, and continue as the medial lemniscus.
- Trochlear and Abducent Nerves: The trochlear nerve arises from the lower midbrain, while the abducent nerve arises from the pons.
Interpeduncular Fossa
The interpeduncular fossa is a rhomboid-shaped space situated between the crus cerebri of the cerebral peduncles. Its boundaries are as follows:
- Anteriorly: the optic chiasma and optic tracts
- Posteriorly: the pons
Contents of the Interpeduncular Fossa
The interpeduncular fossa contains several important structures, which are arranged from anterior to posterior as follows:
- A narrow stalk called the infundibulum, which connects the hypophysis cerebri (pituitary gland) with the tuber cinereum.
- A raised area of grey matter known as the tuber cinereum, located anterior to the mammillary bodies.
- Two small, round structures called mammillary bodies.
- The posterior perforated substance, a layer of grey matter found between the crus cerebri, which is pierced by branches of the posterior cerebral arteries.
- The oculomotor nerve, which emerges just dorsomedially from the corresponding crus.
Additionally, the trochlear nerve runs close to the interpeduncular fossa.
CNS and Brain Stem Nuclei
- The central nervous system (CNS) develops from the neural tube, which is divided horizontally into two regions: the dorsal (sensory) and ventral (motor) areas. This division is marked by the sulcus limitans.
- The dorsal alar plate is responsible for producing sensory nuclei, while the ventral plate generates motor nuclei. These sensory and motor nuclei are kept separate by the sulcus limitans.
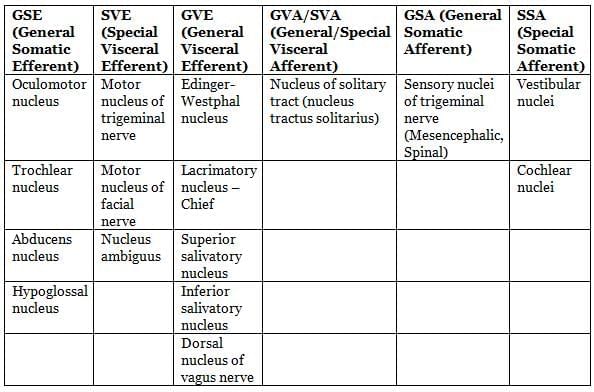
Functional components, nuclei, distribution and functions of cranial nerves.
I. Olfactory Nerve
- Functional Component: Special Visceral Afferent (SVA)
- Nuclei: None (directly connects to olfactory bulb)
- Distribution: Olfactory epithelium in the nasal cavity
- Function: Sense of smell
II. Optic Nerve
- Functional Component: Special Somatic Afferent (SSA)
- Nuclei: None (directly connects to retina)
- Distribution: Retina of the eye
- Function: Vision
III. Oculomotor Nerve
- Functional Components: Somatic Efferent (SE), General Visceral Efferent (GVE)
- Nuclei: Oculomotor nucleus, Edinger-Westphal nucleus
- Distribution:
- SE: All extrinsic eye muscles except lateral rectus and superior oblique
- GVE: Sphincter pupillae and ciliary muscle
- Functions:
- Eye movement
- Pupil constriction and lens accommodation
IV. Trochlear Nerve
- Functional Component: Somatic Efferent (SE)
- Nucleus: Trochlear nucleus
- Distribution: Superior oblique muscle of the eye
- Function: Eye movement
V. Trigeminal Nerve
- Functional Components: Special Visceral Efferent (SVE), General Somatic Afferent (GSA)
- Nuclei:
- SVE: Motor nucleus of trigeminal
- GSA: Chief sensory nucleus, spinal trigeminal nucleus, mesencephalic nucleus
- Distribution:
- SVE: Muscles of mastication
- GSA: Skin of face, mucous membranes of mouth and nose, proprioceptive fibers
- Functions:
- Mandibular movement (mastication)
- Sensation of touch, pain, temperature, and proprioception from face and oral cavity
VI. Abducens Nerve
- Functional Component: Somatic Efferent (SE)
- Nucleus: Abducens nucleus
- Distribution: Lateral rectus muscle of the eye
- Function: Abduction of the eye
VII. Facial Nerve
- Functional Components: General Visceral Efferent (GVE), Special Visceral Efferent (SVE), Special Visceral Afferent (SVA), General Somatic Afferent (GSA)
- Nuclei:
- GVE: Superior salivatory nucleus
- SVE: Motor nucleus of facial nerve
- SVA: Nucleus tractus solitarius
- GSA: Spinal trigeminal nucleus
- Distribution:
- GVE: Submandibular and sublingual salivary glands
- SVE: Muscles of facial expression, stylohyoid, posterior digastric, platysma, stapedius
- SVA: Taste buds in anterior two-thirds of tongue (except vallate papillae)
- GSA: Skin of external ear
- Functions:
- Secretion of saliva
- Facial expression, hyoid elevation, sound modulation (stapedius)
- Taste from anterior two-thirds of tongue
- Sensation from external ear
VIII. Vestibulocochlear Nerve
- Functional Component: Special Somatic Afferent (SSA)
- Nuclei: Cochlear nuclei, vestibular nuclei
- Distribution:
- Cochlear: Organ of Corti in the cochlea
- Vestibular: Receptors in semicircular canals, utricle, and saccule
- Functions:
- Hearing
- Balance and equilibrium
IX. Glossopharyngeal Nerve
- Functional Components: Special Visceral Efferent (SVE), General Visceral Efferent (GVE), General Visceral Afferent (GVA), Special Visceral Afferent (SVA)
- Nuclei:
- SVE: Nucleus ambiguus
- GVE: Inferior salivatory nucleus
- GVA/SVA: Nucleus tractus solitarius
- Distribution:
- SVE: Stylopharyngeus muscle
- GVE: Parotid gland
- GVA: Pharynx, posterior third of tongue
- SVA: Taste buds in posterior third of tongue and vallate papillae
- Functions:
- Larynx elevation
- Saliva secretion
- Sensation (touch, pain, temperature) from pharynx and posterior tongue
- Taste from posterior third of tongue
X. Vagus Nerve
- Functional Components: Special Visceral Efferent (SVE), General Visceral Efferent (GVE), General Visceral Afferent (GVA), Special Visceral Afferent (SVA), General Somatic Afferent (GSA)
- Nuclei:
- SVE: Nucleus ambiguus
- GVE: Dorsal nucleus of vagus
- GVA/SVA: Nucleus tractus solitarius
- GSA: Spinal trigeminal nucleus
- Distribution:
- SVE: Muscles of palate, pharynx, and larynx
- GVE: Smooth muscles and glands of thoracic and abdominal viscera
- GVA: Thoracic and abdominal viscera
- SVA: Taste buds in posterior tongue and epiglottis
- GSA: Skin of external ear
- Functions:
- Movements of palate, pharynx, and larynx
- Motor and secretory control of respiratory and digestive systems; heart inhibition
- General sensation from viscera
- Taste from posterior tongue and epiglottis
- Sensation from external ear
XI. Accessory Nerve
- Functional Components: Special Visceral Efferent (SVE), General Somatic Efferent (GSE)
- Nuclei: Nucleus ambiguus, spinal accessory nucleus (upper cervical spinal cord)
- Distribution:
- SVE: Muscles of palate, pharynx, and larynx
- GSE: Trapezius and sternocleidomastoid muscles
- Functions:
- Movements of palate, pharynx, and larynx
- Head and shoulder movements
XII. Hypoglossal Nerve
- Functional Component: Somatic Efferent (SE)
- Nucleus: Hypoglossal nucleus
- Distribution: All intrinsic and extrinsic tongue muscles (except palatoglossus)
- Function: Tongue movements
The brainstem comprises three regions: the midbrain, pons, and medulla oblongata, housing the nuclei for cranial nerves 3–12. Specifically, the midbrain contains nuclei for cranial nerves 3 and 4, the pons for nerves 5–8, and the medulla for nerves 9–12. Motor nuclei are positioned medially, while sensory nuclei are lateral.
- Motor Nuclei: These are lower motor neurons (LMNs) that innervate head skeletal muscles and are influenced by upper motor neurons (UMNs) via corticobulbar fibers originating in the frontal motor cortex of the cerebrum.
- Cranial Nerve Functions:
- Pure Sensory: Cranial nerves 1, 2, and 8 handle sensory input.
- Pure Motor: Cranial nerves 3, 4, 6, 11, and 12 manage motor functions.
- Mixed (Sensory and Motor): Cranial nerves 5, 7, 9, and 10 perform both sensory and motor roles.
Types of Fibers:
- General Somatic Efferent (GSE): Transmit motor signals to skeletal muscles throughout the body.
- Special Visceral Efferent (SVE): Control muscles of the head and neck derived from pharyngeal arches, including muscles for mastication (cranial nerve 5), facial expression (cranial nerve 7), and palate, pharynx, and larynx (speech/swallowing, cranial nerves 9, 10, 11 via nucleus ambiguus).
- General Visceral Efferent (GVE): Conduct motor impulses to smooth muscle, cardiac muscle, and glands (part of the autonomic nervous system, ANS).
- General Somatic Afferent (GSA): Relay sensations like touch, pain, temperature, and proprioception from the body to the central nervous system (CNS).
- Special Visceral Afferent (SVA): Transmit taste sensations to the CNS.
- General Visceral Afferent (GVA): Carry sensory input from visceral organs, such as pressure from the carotid sinus.
- Special Somatic Afferent (SSA): Convey special sensory information for vision, hearing, and balance.
SVE Details: These fibers innervate muscles from pharyngeal arches:
- Arch I: Muscles of mastication (cranial nerve 5).
- Arch II: Muscles of facial expression (cranial nerve 7).
- Arches III, IV, VI: Muscles of the palate, pharynx, and larynx (cranial nerves 9, 10, 11, via nucleus ambiguus).
GVE and GVA (ANS-related):
- GVE: Motor fibers regulate cardiac muscle, smooth muscle, and glands.
- GVA: Sensory fibers transmit visceral sensations, such as angina or colicky pain, to the CNS.
Nucleus Tractus Solitarius (NTS)
The Nucleus Tractus Solitarius (NTS) is a sensory region in the medulla oblongata that plays a crucial role in processing various visceral sensory information. It receives input from the solitary tract, which transmits signals from the facial, glossopharyngeal, and vagus nerves.
The NTS contains two main types of neural columns:
- SVA (Special Visceral Afferent). This column is responsible for processing taste sensations and is located in the upper part of the nucleus.
- GVA (General Visceral Afferent). This column handles sensations such as pressure from the carotid sinus, chemical signals from the carotid body, and information from the cardio-respiratory and gastrointestinal systems. It is situated in the lower part of the nucleus.
The NTS is involved in several reflex actions, including:
- The gag reflex
- The carotid sinus reflex
- The aortic reflex
- The cough reflex
- Baroreceptor and chemoreceptor reflexes
- Various respiratory reflexes
- Reflexes regulating gastrointestinal motility and secretion
Information from the NTS is relayed to various brain regions, including:
- The paraventricular nucleus of the hypothalamus
- The central nucleus of the amygdala
- Other brainstem nuclei, such as the parabrachial area, locus coeruleus, and dorsal raphe nucleus
Nucleus Ambiguus
- Contains lower motor neurons for cranial nerves 9, 10, and 11 (cranial part).
- Part of the special visceral efferent (SVE) column, innervating pharyngeal arch muscles of the palate, pharynx, larynx (for speech and swallowing), and upper esophagus.
- Its "external formation" includes cholinergic preganglionic parasympathetic neurons regulating the heart.
- Located in the upper medulla oblongata, within the medullary reticular formation, posterior to the inferior olivary nucleus and posteromedial to the olive.
- Receives upper motor neuron input through the corticobulbar tract.
- Lesions cause:
- Impaired speech and swallowing (nasal speech, dysphagia, dysphonia).
- Uvula deviation to the contralateral side due to unopposed action of unaffected contralateral muscles.
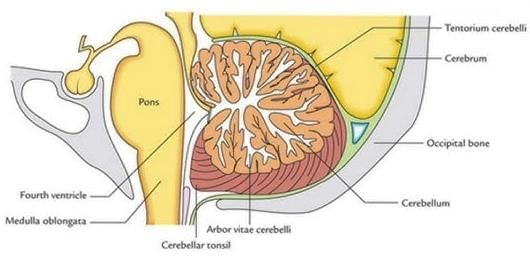
Cerebellum
Embryological Origin: The cerebellum develops from the rhombic lips, thickened regions of the neural tube’s alar plates. Its rostral portion originates from the caudal mesencephalon.
Location and Structure: Situated in the hindbrain (metencephalon) within the posterior cranial fossa, the cerebellum lies posterior to the fourth ventricle, pons, and medulla. It is separated from the occipital lobes of the cerebrum by the tentorium cerebelli, a dura mater layer. The cerebellum consists of two hemispheres and a central vermis (midline zone). Its outer layer, the cerebellar cortex, is composed of tightly folded gray matter forming folia (gyri) and sulci. Beneath this lies white matter, primarily myelinated nerve fibers, resembling a tree-like pattern (arbor vitae) in cross-section. Four deep cerebellar nuclei (gray matter) are embedded within the white matter.
Structural Divisions: The cerebellum is divided into three lobes:
- Anterior lobe: Located above the primary fissure.
- Posterior lobe: Below the primary fissure.
- Flocculonodular lobe: Below the posterior fissure.
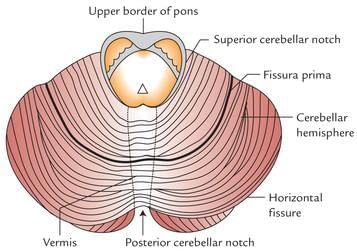
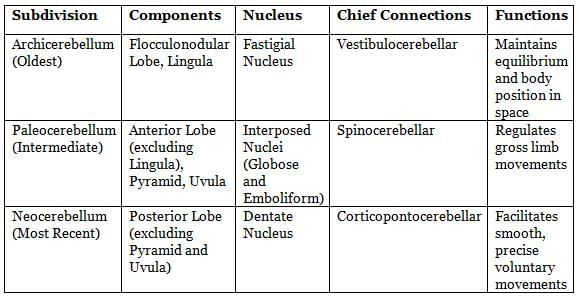
Functional Divisions (based on medial-to-lateral organization):
- Spinocerebellum (Paleocerebellum):
- Location: Medial zone of the anterior and posterior lobes.
- Function: Fine-tunes body and limb movements.
- Inputs: Receives proprioceptive signals from the spinal cord’s dorsal columns (including the spinocerebellar tract), cranial trigeminal nerve, and visual/auditory systems.
- Outputs: Projects to deep cerebellar nuclei, which connect to the cerebral cortex and brainstem, modulating descending motor pathways.
- Cerebrocerebellum (Neocerebellum):
- Location: Lateral regions.
- Inputs: Receives signals from the cerebral cortex (particularly the parietal lobe) via the pontine nuclei (cortico-ponto-cerebellar pathways).
- Outputs: Sends fibers to the ventrolateral thalamus, which connects to motor areas of the premotor and primary motor cortex, and to the red nucleus.
- Vestibulocerebellum (Archicerebellum):
- Location: Flocculonodular lobe and vermis.
- Function: Primarily regulates balance and spatial orientation.
- Inputs: Mainly connected to the vestibular nuclei, with additional visual and sensory inputs.
- Role: As the oldest cerebellar region, it supports equilibrium and spatial coordination.
Subdivisions of Vermis and Cerebellar Hemisphere
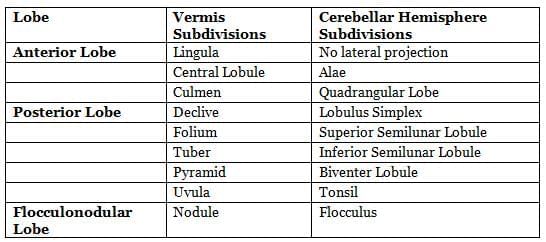
Morphological Subdivisions, Components, Nuclei, Connections, and Functions
The cerebellar circuit primarily involves two key neuron types: Purkinje cells and granule cells. Three types of axons are also critical: mossy fibers and climbing fibers (afferent inputs to the cerebellum) and parallel fibers (axons of granule cells). The cerebellum features two main pathways, initiated by mossy and climbing fibers, both ultimately connecting to the deep cerebellar nuclei.
The cerebellar cortex is organized into three layers with five cell types:
- Molecular layer (outermost): Contains two inhibitory (GABAergic) interneurons—stellate and basket cells—and parallel fibers that intersect Purkinje cell dendrites at right angles.
- Purkinje cell layer (middle): Consists of Purkinje cells.
- Granular layer (inner): Includes granule cells and Golgi cells.
Deep cerebellar nuclei, embedded in the white matter at the cerebellum’s core, are arranged from lateral to medial as dentate, emboliform, globose, and fastigial. The dentate nucleus, the largest and most evolutionarily recent, interacts solely with the lateral cerebellar cortex. The flocculonodular lobe, unlike other cerebellar cortex regions, projects to the vestibular nuclei rather than the deep nuclei. These nuclei receive collateral inputs from mossy and climbing fibers and inhibitory signals from Purkinje cells. Except for minor projections to the vestibular nuclei, the deep nuclei are the cerebellum’s sole output sources.
Climbing fibers (olivocerebellar fibers) originate from the contralateral inferior olivary nucleus in the brainstem, travel through the inferior cerebellar peduncle, and target Purkinje cells. Each climbing fiber provides collaterals to the deep nuclei before branching into approximately 10 terminals, each synapsing with a single Purkinje cell. The inferior olive, located in the medulla oblongata, receives inputs from the spinal cord, brainstem, and cerebral cortex but directs all its output to the cerebellum.
Mossy fibers, afferent inputs from sources like the pontine nuclei, spinal cord, and vestibular nuclei, form excitatory synapses with granule cells and deep cerebellar nuclei. In the granular layer, mossy fibers create enlargements called rosettes, which connect with granule cell dendrites within structures called glomeruli, also involving Golgi cell axons. Mossy fibers project directly to the deep nuclei and indirectly via the pathway: mossy fibers → granule cells → parallel fibers → Purkinje cells → deep nuclei.
Cerebellar Pathways:
- Mossy and climbing fibers, excitatory afferents, enter via the cerebellar peduncles and synapse directly or indirectly (via granule cells) with Purkinje cells.
- Purkinje cell axons, which are inhibitory (GABAergic), are the only efferents from the cerebellar cortex, targeting and inhibiting the deep cerebellar nuclei (dentate, interposed, fastigial) in the medulla.
- Efferents from the deep nuclei travel through the superior cerebellar peduncle to the contralateral ventral lateral and ventral anterior thalamic nuclei, ultimately influencing the contralateral cerebral cortex (precentral gyrus). Upper motor neurons in the cerebrum then affect contralateral lower motor neurons in the spinal cord via the corticospinal tract.
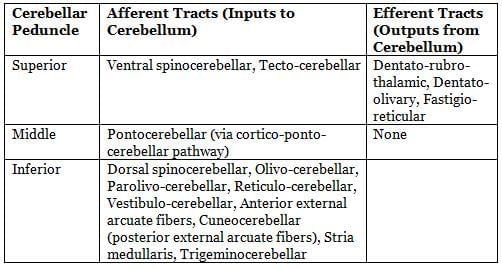
Cerebellar Peduncles:The cerebellum connects to the brainstem via three paired peduncles: superior, middle, and inferior.
- Superior cerebellar peduncle: Primarily carries output from the deep nuclei to the cerebral cortex, targeting upper motor neurons.
- Middle cerebellar peduncle: The largest, it connects to the pons, receiving inputs from the cerebral cortex via the cortico-ponto-cerebellar tract.
- Inferior cerebellar peduncle: Receives afferent inputs from the spinal cord, vestibular nuclei, and tegmentum, including all modulatory input from the inferior olivary nucleus via climbing fibers. Its efferents project to the vestibular nuclei and reticular formation.
Cerebellar Pathways and Functions
Neural Tracts:
- Spinocerebellar Tract: Originates in the spinal cord and terminates in the same-sided cerebellum, transmitting unconscious proprioceptive information about muscle fiber length and tension from the trunk and lower limbs.
- Cuneocerebellar Tract: Carries proprioceptive signals from the upper limbs and neck to the ipsilateral cerebellum via posterior external arcuate fibers.
- Dentato-rubro-thalamic Tract: Connects the dentate nucleus to the thalamus (ventral intermediate nucleus), with collaterals to the red nucleus, relaying information to the cerebral cortex.
- Cortico-ponto-cerebellar Tract: Links the cerebral cortex to the contralateral cerebellum. Second-order pontocerebellar fibers cross in the pons, travel through the middle cerebellar peduncles, and reach the opposite cerebellar hemisphere.
- Olivocerebellar Tract: Arises from the olivary nucleus, decussates in the raphe nucleus, and travels through or around the opposite olive via internal arcuate fibers to enter the inferior cerebellar peduncle, terminating as climbing fibers on Purkinje cells in the contralateral cerebellar hemisphere.
Arterial Supply:The cerebellum is supplied by three paired arteries:
- Superior Cerebellar Artery (SCA): Supplies the upper cerebellum.
- Anterior Inferior Cerebellar Artery (AICA): Supplies the anterior undersurface of the cerebellum.
- Posterior Inferior Cerebellar Artery (PICA): Divides into medial and lateral branches. The medial branch extends to the cerebellar notch between hemispheres, while the lateral branch supplies the undersurface up to the lateral border, where it connects with the AICA and SCA.
Functions:
- The cerebellum coordinates voluntary motor activity, regulates posture, balance, and muscle tone, and supports motor learning.
- It does not initiate movement but ensures coordination, precision, and timing.
- Cerebellar lesions cause ataxia, leading to abnormal gait, balance issues, and impaired coordination without paralysis. Symptoms include disrupted fine movements, posture, and motor learning.
Effects of Cerebellar Damage:
- Flocculonodular Lobe Damage: Results in loss of equilibrium, irregular gait, and a wide stance due to balance difficulties.
- Lateral Zone Damage: Impairs skilled voluntary movements, causing errors in force, direction, speed, and amplitude. Symptoms include hypotonia, dysmetria, dysdiadochokinesia, impaired check reflex, intention tremor, and dysarthria.
- Midline Damage: Affects whole-body movements.
- Lateral Damage: Disrupts fine hand or limb movements.
- Cerebellar Ataxia: Upper cerebellar damage primarily causes gait and leg coordination issues, while lower damage affects arm and hand coordination, speed, and accuracy.
SC - Vertebral Canal
- The number of spinal segments corresponds to the number of vertebrae in the thoracic, lumbar, and sacral regions.
- In the cervical region, there is one additional segment compared to the number of vertebrae.
- In the coccygeal area, there is one segment for four coccygeal vertebrae.
- As a result, the spinal cord comprises 31 spinal segments. 8 cervical, 12 thoracic, 5 lumbar, 5 sacral, and 1 coccygeal.
Spinal Nerve Roots
- Due to the spinal cord being shorter than the vertebral column, the length and angle of spinal nerve roots increase gradually from top to bottom.
- In the upper cervical region, spinal nerve roots are short and run almost horizontally. In contrast, lumbar and sacral nerve roots are longer and run at a steep angle, nearly vertically.
- At the thoracic, lumbar, sacral, and coccygeal levels, each numbered nerve exits the vertebral canal by passing below its corresponding vertebra (e.g., the L4 nerve exits between L4 and L5).
- In the cervical region, nerves C1–7 exit above their corresponding vertebrae. C1 exits at the atlanto-occipital joint (known as the suboccipital nerve ). The last pair of cervical nerves does not have a matching vertebra, with C8 exiting between the 7th cervical and 1st thoracic vertebrae.
- The first and second cervical spinal roots are short and run almost horizontally to exit the vertebral canal. From the third to the eighth cervical levels, the roots slope downward at an angle. Lumbar, sacral, and coccygeal roots descend at a greater angle to exit.
Approximate Vertebral Levels of Spinal Cord Segments
- In the cervical region, the tip of a vertebral spinous process corresponds with the next spinal cord segment (e.g., the sixth cervical spine is opposite the seventh spinal segment).
- At upper thoracic levels, the tip of a vertebral spine aligns with the cord two segments lower (e.g., the fourth spine is level with the sixth segment). In the lower thoracic region, the difference is three segments (e.g., the tenth thoracic spine is aligned with the first lumbar segment).
- The eleventh thoracic spine overlays the third lumbar segment, and the twelfth is opposite the first sacral segment.
Cervical and Lumbar Enlargements
- Cervical Enlargement: This region of the spinal cord provides axons to the brachial plexus, which innervates the upper limbs. The cervical enlargement extends from the C3 to T2 segments, with the largest circumference at the C6 segment.
- Lumbar Enlargement: The lumbar enlargement supplies axons to the lumbar and sacral plexus for the lower limbs. This enlargement extends from the L1 to S3 segments, with equivalent vertebral levels being the last four thoracic vertebrae (T9–T12). The largest circumference is at the lower part of the T12 vertebra, and it is protected by the last four thoracic vertebrae (T9–T12).
Filum Terminale
- The upper 15 cm of the filum terminale (pial part) is covered by dural and arachnoid meninges and reaches the lower border of the second sacral vertebra. The lower 5 cm (dural part) fuses with the dura mater and then both descend to the back of the first coccygeal vertebral segment.
Spinal Meninges Spaces
- Epidural Space: This space is located between the periosteum lining the bony wall of the vertebral canal and the spinal dura mater. It contains fat (loose connective tissue) and internal vertebral venous plexuses. Below the L2 vertebra, the epidural space encases the roots of spinal nerves.
- Subarachnoid Space: Also known as the leptomeningeal space, this naturally occurring space is between the arachnoid mater and pia mater. It contains cerebrospinal fluid (CSF), radicular, segmental, medullary, and spinal arteries, veins, and arachnoid trabeculae.
Spinal Meninges and Ligamentum Denticulatum
- The spinal meninges, consisting of the dura mater, arachnoid mater, and pia mater, protect the spinal cord and nerve roots. The ligamentum denticulatum, made of pia mater, attaches to the dura mater and lies on each side between the dorsal and ventral nerve roots, forming narrow, ribbon-like transparent bands.
- The lateral margin of each ligamentum denticulatum sends 21 teeth-like projections that pass through the subarachnoid space and the arachnoid mater to attach to the inner surface of the dural tube between the points where two adjacent spinal nerves emerge.
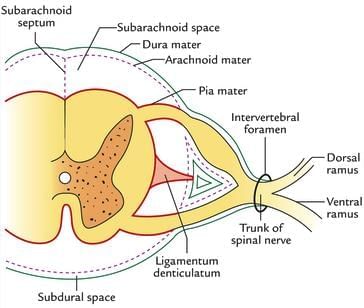
The ligamenta denticulata plays a crucial role in stabilizing the spinal cord within the subarachnoid space. This ligament consists of a series of teeth-like projections that anchor the spinal cord, preventing excessive movement and ensuring its proper positioning. The first tooth of the ligamenta denticulata is located above the rim of the foramen magnum, while the last tooth is situated between the exiting twelfth thoracic and first lumbar spinal nerves.
Herniated Disc Effects
A herniated disc can lead to several neurological deficits due to the compression of nerve roots. The specific effects depend on which nerve root is compressed. Here are the details of the affected dermatomes, muscles, weaknesses, and involved nerves and reflexes for different levels of nerve root compression:
C4 and C5:
- Dermatome Affected: Lateral surface of the arm
- Muscles Affected: Deltoid
- Weakness: Abduction of arm
- Nerve Involved: Axillary nerve
- Reflex:. biceps jerk
C5 and C6:
- C6 Dermatome: Lateral surface of the forearm, thumb, and index finger
- Muscles Affected: Biceps, Brachialis, Brachioradialis
- Weakness: Flexion of forearm, supination/pronation
- Nerve Involved: Musculocutaneous nerve
- Reflexes:. biceps reflex, ↓ brachioradialis (supinator) reflex
C6 and C7:
- Dermatome Affected: Middle finger
- Muscles Affected: Triceps, Wrist extensors
- Weakness: Extension of forearm, extension of wrist
- Nerve Involved: Radial nerve
- Reflex:. triceps jerk
L3 and L4:
- Dermatome Affected: Medial surface of the leg
- Muscles Affected: Quadriceps
- Weakness: Extension of knee
- Nerve Involved: Femoral nerve
- Reflex:. knee jerk
L5 and S1:
- Dermatome Affected: Lateral surface of leg, dorsum of foot, big toe
- Muscles Affected: Tibialis anterior, extensor hallucis longus, extensor digitorum longus
- Weakness: Dorsiflexion of ankle (patient cannot stand on heels), extension of toes
- Nerve Involved: Common fibular
- Reflex: No reflex loss
Heel:
- Dermatome Affected: Little toe
- Muscles Affected: Gastrocnemius, soleus
- Weakness: Plantar flexion of ankle (patient cannot stand on toes), flexion of toes
- Nerve Involved: Tibial nerve
- Reflex:. ankle jerk
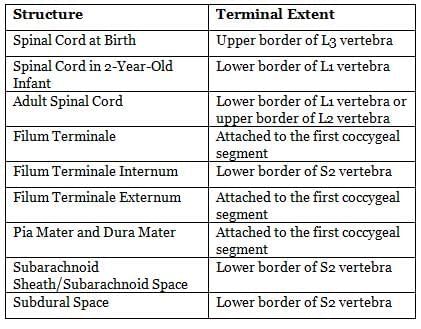
Spinal Cord Termination
The spinal cord occupies the upper two-thirds of the vertebral canal. It connects to the medulla oblongata at the top and ends at the conus medullaris, situated at the lower edge of the L1 vertebra.
Developmental Changes
- Initially, during growth, the vertebral column elongates more rapidly than the spinal cord, creating a disparity between the spinal cord segments and their corresponding vertebrae.
- At week 8 of development, both the vertebral column and the spinal cord are of equal length, with the spinal cord terminating at the lower border of the L3 vertebra.
- Upon birth, the conus medullaris is positioned at the top of the third lumbar vertebra.
- As the spinal column continues to grow, the conus medullaris typically migrates to its adult position at the L1 vertebra by the age of 2.
- In adult individuals, the conus medullaris is found at the lower border of the L1 vertebra.
The disparity in growth rates between the spinal cord and vertebral column leads to the formation of the cauda equina, which consists of the posterior and anterior nerve roots (ranging from L3 to the coccygeal region) that extend below the conus medullaris. Additionally, this uneven growth results in the filum terminale, a structure that anchors the spinal cord to the dura mater and the coccyx.
As the spinal cord ascends during development, the angles of the spinal nerve roots become more pronounced, slanting from above downwards. The spinal cord, along with its blood vessels and nerve roots, is protected within a meningeal sheath, also known as the theca, which extends from the foramen magnum to the level of the second sacral vertebra in adults. Below this level, the dura mater continues as a slender cord called the filum terminale externum, which merges with the periosteum at the back of the first coccygeal segment.
Filum Terminale
- The filum terminale is a connective tissue strand approximately 20 cm long, originating from the tip of the conus medullaris.
- The upper 15 cm of this strand, referred to as the filum terminale internum, is located within the dural and arachnoid meninges, extending to the lower border of the second sacral vertebra.
- The remaining 5 cm, known as the filum terminale externum, connects with the dura mater and descends to the back of the first coccygeal vertebra.
- The filum terminale is continuous above with the spinal pia mater.
Structure/Space
Vascular Supply of the Spinal Cord
Arterial Supply
Blood Supply Overview: The spinal cord receives its blood supply from one main artery at the front and two at the back, originating from the vertebral artery in the skull and ending in a network around the conus medullaris.
Anterior Spinal Artery:. central vessel formed by the joining of two vertebral arteries, running down the front of the spinal cord.
Posterior Spinal Arteries: Two arteries that come from the vertebral artery (or the posterior inferior cerebellar artery) and travel down the back sides of the spinal cord.
- Segmental Arteries: These arteries branch from the vertebral, deep cervical, intercostal, and lumbar arteries in a top-to-bottom order. They enter the vertebral canal through openings between the vertebrae and connect with branches of the main arteries to create a pial plexus on the surface of the spinal cord.
- Great Anterior Radiculo-medullary Artery (of Adamkiewicz): The largest artery supplying the front of the spinal cord, usually found on the left side. It may come from branches of the lower posterior intercostal arteries (T9–11), the subcostal artery (T12), or, less commonly, from the upper lumbar arteries (L1 and L2). This artery may supply most of the lower two-thirds of the spinal cord.
Venous Drainage
- Intramedullary Veins: Veins inside the spinal cord that drain into a surrounding network of surface veins known as the coronal plexus (venous plexus of the pia mater).
- Coronal Plexus:. network of surface veins that includes six winding vertical channels:
- Anterior and Posterior Spinal Veins: Also known as anterior and posterior median veins.
- Other Veins: Four additional veins alongside the front and back nerve roots.
- Drainage Connections: These veins connect easily and drain into the cerebellar veins, cranial sinuses, and mainly into segmental medullary veins.
- Segmental Veins: Veins that flow into the intervertebral veins and then into the external vertebral venous plexuses, including the caval and azygos systems.
Neural Pathways
Neural pathways consist of a series of connected neurons that facilitate the transmission of signals within the central nervous system (CNS). These pathways can involve either a single axon or a sequence of axons and are known by various terms such as tract, lemniscus, capsule, and fasciculus. Neural pathways are organized into ascending and descending pathways.
Sensory modalities refer to the different types of sensory information that can be perceived, and they include both special senses and general senses.
Special Senses:These include:
- Olfaction: The sense of smell.
- Vision: The sense of sight.
- Taste: The sense of taste.
- Hearing: The sense of hearing.
- Vestibular Function: The sense responsible for balance.
General Senses:These include:
- Touch: The perception of physical contact with the skin.
- Pressure: The perception of pressure applied to the skin.
- Vibration: The perception of vibrations through the skin.
- Pain: The perception of pain sensations.
- Thermal Sensation: The perception of temperature changes.
- Proprioception: The awareness of body position and movement.
Afferent information, which includes sensory data from specialized sense organs, is transmitted to the brain via cranial nerves for special senses. For general senses, signals from the trunk and limbs are relayed to the spinal cord through spinal nerves, while signals from the head reach the brain through cranial nerves.
Generally, ascending sensory pathways for general senses consist of three neurons that extend from peripheral receptors to the opposite side of the cerebral cortex. These neurons are referred to as first, second, and third-order neurons.
- First-order neurons have sensory endings located peripherally, with cell bodies found in dorsal root ganglia or sensory ganglia associated with specific cranial nerves. Their axons enter the CNS through spinal or cranial nerves and connect with the cell bodies of second-order neurons on the same side.
Pain, temperature, and coarse touch information from the trunk and limbs are transmitted by the spinothalamic tract, which is primarily responsible for pain and temperature sensations. Similar fibers from the head terminate in the trigeminal sensory nucleus of the brainstem.
Proprioceptive information and fine touch sensations from the trunk and limbs travel upward on the same side of the spinal cord as part of the dorsal column-medial lemniscal system. A similar projection exists for afferents from the head.
Major Ascending Tracts in the Spinal Cord
Lateral Spinothalamic Tract
- Origin: Lateral white column of the spinal cord
- Pathway: First-order neurons synapse in the posterior horn of the spinal cord on the opposite side. Second-order neurons project to the ventral posterolateral nucleus of the thalamus.
- Function: Carries pain and temperature sensations from the opposite side of the body.
Anterior Spinothalamic Tract
- Origin: Anterior white column of the spinal cord
- Pathway: First-order neurons synapse in the posterior horn of the spinal cord on the opposite side. Second-order neurons project to the thalamus.
- Function: Carries light touch, pressure, tickle, and itch sensations from the opposite side of the body.
Spinotectal Tract
- Origin: Lateral white column of the spinal cord
- Pathway: First-order neurons synapse in the posterior horn of the spinal cord. Second-order neurons project to the superior colliculus of the midbrain.
- Function: Facilitates head and eye movements towards the source of stimulation.
Spinocerebellar Tracts (Anterior and Posterior)
- Origin: Lateral white column of the spinal cord (superficially)
- Pathway: First-order neurons synapse in the posterior horn of the spinal cord on the same side. Second-order neurons project to the cerebellum.
- Function: Carries unconscious proprioceptive information (kinesthesia) to the cerebellum.
Fasciculus Gracilis and Fasciculus Cuneatus (Tracts of Gall and Burdach)
- Origin: Posterior white column of the spinal cord
- Pathway: First-order neurons synapse in the dorsal root ganglia of spinal nerves on the same side. Second-order neurons project to the nucleus gracilis and nucleus cuneatus in the medulla on the same side.
- Function: Carries joint sense, vibration sense, two-point discrimination, stereognosis, and conscious kinesthesia to the cerebrum.
Dorsal Column-Medial Lemniscal System (DC-MLS)
The Dorsal Column-Medial Lemniscal System (DC-MLS) is responsible for carrying various sensory modalities, including:
- Fine (Discriminative) Touch
- Pressure
- Vibration
- Conscious Proprioception
- Stereognosis
First Order Neurons
- Located in the dorsal root ganglion.
- Transmit information ipsilaterally (same side) through the dorsal column, specifically the fasciculus cuneatus and gracilis.
- Connect with second order neurons in the gracile and cuneate nuclei of the caudal medulla.
Second Order Neurons
- Found in the gracile and cuneate nuclei of the caudal medulla.
- Produce axons called internal arcuate fibers, which decussate (cross over) and form the medial lemniscus.
Medial Lemniscus
- The medial lemniscus carries the sensory information contralaterally (to the opposite side) and ascends through the brainstem.
- It ends in the ventral posterolateral (VPL) nucleus of the thalamus.
Third Order Neurons
- Located in the VPL nucleus of the thalamus.
- Extend through the posterior limb of the internal capsule to the primary somatosensory cortex in the postcentral gyrus (Brodmann’s areas 3, 1, and 2).
|
42 docs|7 tests
|
FAQs on Neuroanatomy - 3 Chapter Notes - Anatomy - NEET PG
| 1. What is the role of the medulla oblongata in the central nervous system? |  |
| 2. Can you explain the structure and significance of the interpeduncular fossa? |  |
| 3. What are the key features of the dorsal column-medial lemniscal system (DC-MLS)? |  |
| 4. How does the vascular supply of the spinal cord function? |  |
| 5. What are the main neural pathways found in the brainstem? |  |















