Bronchopneumonia and ARI | Medical Science Optional Notes for UPSC PDF Download
| Table of contents |

|
| Acute Respiratory Insufficiency (ARI) |

|
| Etiology-Pneumonia |

|
| Pneumonia-Management |

|
| Bronchopneumonia/ARI-Repeats |

|
Acute Respiratory Insufficiency (ARI)

In Children Below 2 Months: Indicators of Severe Disease
- Fever (38°C or more)
- Convulsions
- Abnormally Sleepy or Difficult to Wake
- Stridor in a Calm Child
- Wheezing
- Not Feeding
- Tachypnea
- Chest Indrawing
- Altered Sensorium
- Central Cyanosis
- Grunting or Apneic Spells
- Distended Abdomen
Management for Severe Disease
- Children displaying any of the above signs should be referred to a hospital for admission.
- Treatment involves parenteral administration of ampicillin and gentamicin.
- Supportive care measures are also essential.
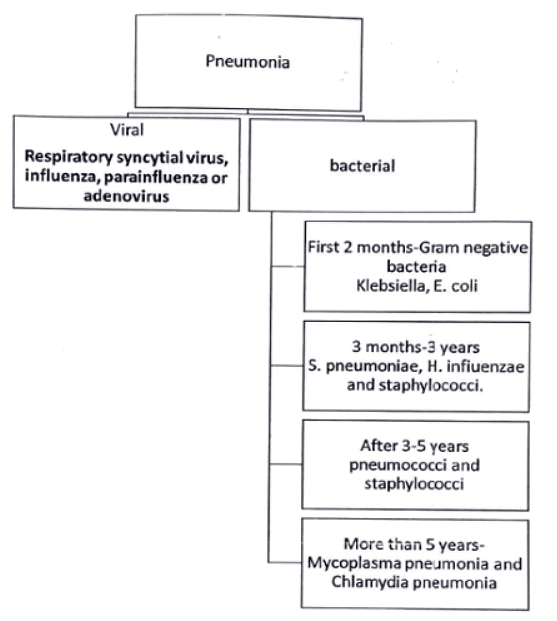
Etiology-Pneumonia
- The common bacteria causing LRTI in preschool children include H. influenzae, S. pneumoniae and staphylococci. All these agents are sensitive to antibacterials like cotrimoxazole.
- Gram-negative organisms cause pneumonia in early infancy, severe malnutrition and immunocompromised children.
- Pneumocystis jiroveci, histoplasmosis and coccidioidomycosis may cause pneumonia in immunocompromised children.
- Other causes of pneumonia include ascaris, aspiration of food, oily nose drops, liquid paraffin and kerosene poisoning.
- The etiology remains unknown in one-third of cases of pneumonia.
Pneumonia-Management
Diagnosis: Chest X-ray
- Viral Pneumonia:
- Hyperinflation with bilateral interstitial infiltrates and peribronchial cuffing.
- Pneumococcal Pneumonia:
- Confluent lobar consolidation.
- Complete blood picture (CBP).
- Leucocytosis Types:
- Lymphocytic leucocytosis (<20,000/mm³) indicates viral pneumonia.
- Neutrophilic leucocytosis (15,000-40,000/mm³) indicates bacterial pneumonia.
- Inflammatory Markers:
- ESR/CRP/Procalcitonin raised.
- Atypical pneumonia profile (RNA/DNA assay) for mycoplasma, pertussis, and various viruses.
- Culture and Assays:
- Blood, pleural fluid, and sputum culture.
- Cold agglutinin assay for M. Pneumoniae.
Antibiotics
- Viral Pneumonia:
- Antibiotics may be withheld, especially for mildly ill patients.
- Bacterial Pneumonia:
- High doses of amoxicillin (80-90 mg/kg/24 hr) are the drug of choice.
- Alternatives include cefuroxime axetil, amoxicillin/clavulanate, or macrolide antibiotics like azithromycin for certain cases.
- Staphylococcal Pneumonia:
- If suspected (pneumatoceles, empyema), include vancomycin or clindamycin in initial therapy.
- Duration:
- Antibiotics generally continued until the patient is afebrile for 72 hr, with a total duration of at least 10 days (or 5 days with azithromycin).
Management of Complications
- Lung Abscess:
- Mainly due to anaerobic infection.
- Prolonged antibiotic therapy.
- Minimally invasive CT-guided percutaneous aspiration techniques used if abscesses persist.
- Empyema:
- Tube thoracostomy drainage.
- Intrapleural fibrinolytic therapy (urokinase, streptokinase, tissue plasminogen activator).
- Selected video-assisted thoracoscopy for debridement or lysis.
- Parapneumonic Effusion:
- Aim: Sterilize pleural fluid and restore normal lung function.
- WHO recommends chloramphenicol administration for a total of 4 weeks.
- Necrotising Pneumonia and Pneumatoceles:
- Immediate administration of intravenous antistaphylococcal drugs.
- Treatment depends on methicillin resistance incidence; vancomycin is used if resistance is over 20%.
- Pneumatoceles may spontaneously disappear, but complicated cases may require image-guided catheter drainage or surgical excision.
Supportive Therapy
- Oxygen Administration: Recommended for severe CAP with low chest indrawing or a respiratory rate >70 breaths/min, and all children with very severe CAP.
- Fluid Therapy: Mandatory for severe CAP as affected children may struggle to maintain fluid intake.
- Physiotherapy: Chest physiotherapy is used to evacuate inflammatory exudates, clear tracheobronchial secretions, reduce airway resistance, enhance gas exchange, and ease breathing.
Bronchopneumonia/ARI-Repeats
Q1: Describe the diagnostic categories for acute respiratory infections and pneumonia as per WHO classification. Outline the management of severe pneumonia. (2010)
Q2: A 2-year- old boy was brought to you with cough and fever for 3 days. On examination, the respiratory rate was 46 per minute along with lower chest in drawing. Classify the illness of this child as per. IMNCI guidelines. Outline the treatment for this child. Enumerate the general danger signs you will ask or look for in this child to assess the severity of illness. (2013)
Q3: Enumerate the common causes of community-acquired pneumonia in under-five children. (2014)
Q4: A one-year-old, previously healthy child presents with fever, cold and cough for three days. Mother complains of whistling sound during breathing. There is no history of similar episodes in the past. Examination reveals tachypnea, audible wheeze and hyper inflated chest. His oxygen saturation is 94%. (2016)
(i) What is the most likely diagnosis and what are the probable micro-organisms causing this condition?
(ii) Classify the severity of disease in this patient.
(iii) Outline the principles of management of this child.
Q5: A 10-month-old infant having watery nasal discharge for the last 2 days developed rapid breathing, chest retraction and decreased feeding over the last one day. (2018)
(i) What is the likely diagnosis in this patient?
(ii) Enumerate the microbiological agents for this condition.
(iii) Discuss the investigations and management of this condition.
|
7 videos|219 docs
|
FAQs on Bronchopneumonia and ARI - Medical Science Optional Notes for UPSC
| 1. What is acute respiratory insufficiency and what is its most common cause? |  |
| 2. How is pneumonia managed in patients with ARI? |  |
| 3. What is bronchopneumonia and how does it relate to ARI? |  |
| 4. Can bronchopneumonia and ARI reoccur? |  |
| 5. Are there any preventive measures that can be taken to reduce the risk of ARI and bronchopneumonia? |  |

|
Explore Courses for UPSC exam
|

|

















