Cesarean section | Medical Science Optional Notes for UPSC PDF Download
| Table of contents |

|
| Cesarean section-indications |

|
| Peripartum hysterectomy indications |

|
| Cesarean section-Choice of incision |

|
| Trial of Labour |

|
| Cesarean section-Repeats |

|
Cesarean section-indications
11 possible reasons for the continued increase in the cesarean rates
- A decrease in the overall number of births is contributing to a higher percentage of deliveries occurring in first-time mothers, who have an elevated risk of cesarean section.
- The advancing average age of mothers, particularly among first-time mothers, is linked to a greater likelihood of cesarean deliveries.
- The widespread use of electronic fetal monitoring, associated with a higher cesarean rate compared to intermittent monitoring, is a factor. Concerns over abnormal fetal heart rate tracings often lead to unnecessary cesarean deliveries.
- Cesarean deliveries are now the preferred method for most breech presentations.
- Forceps and vacuum deliveries are less common, contributing to the increased cesarean rate.
- The rising trend in labor induction, especially in first-time mothers, is associated with an elevated cesarean risk.
- The surge in obesity rates significantly raises the likelihood of cesarean deliveries.
- Cesarean rates for women with preeclampsia have risen, while induction rates for this group have declined.
- Vaginal birth after cesarean (VBAC) rates have decreased, with elective cesarean deliveries becoming more common for various reasons, such as concerns about pelvic floor injury, medically indicated preterm births, fetal injury reduction, and maternal preference.
- Malpractice concerns related to fetal injury during both spontaneous and assisted vaginal deliveries continue to contribute to the overall cesarean delivery rate.
- The escalation in cesarean delivery rates is also influenced by the significant impact of malpractice litigation related to fetal injuries during both natural and assisted vaginal deliveries. Legal concerns and the fear of potential complications leading to fetal harm contribute significantly to the decision-making process, encouraging healthcare providers to opt for cesarean deliveries as a precautionary measure to reduce the risk of litigation and associated liabilities. This legal aspect plays a notable role in shaping the prevailing cesarean delivery rate.
Cesarean section-indications
Maternal
- Previous cesarean delivery
- Irregular placental attachment
- Maternal preference for cesarean delivery
- Past classical hysterotomy
- Uncertain uterine scar type
- Uterine incision separation
- Previous extensive myomectomy
- Obstructive mass in the genital tract
- Invasive cervical cancer
- Prior trachelectomy
- Permanent cervix closure
- History of pelvic reconstructive surgery
- Pelvic abnormality
- Infections like HSV or HIV
- Cardiac or pulmonary conditions
- Cerebral aneurysm or arteriovenous malformation
- Underlying health issues requiring simultaneous abdominal surgery
- Emergency cesarean delivery near the time of maternal death.
More than 85 percent of these operations are performed for four reasons—prior cesarean delivery, dystocia, fetal jeopardy, or abnormal fetal presentation.
A resuscitative hysterotomy, also referred to as a perimortem Caesarean section or perimortem Caesarean delivery, is a hysterotomy performed to resuscitate a woman in middle to late pregnancy who has entered cardiac arrest.
Cesarean section-indications

Indications of Classical cesarean section
- Encountering a densely adhered bladder due to a previous surgery.
- Presence of a leiomyoma in the lower uterine segment.
- Invasion of the cervix by cancer.
- Inability to safely access the lower uterine segment due to significant maternal obesity.
- Placenta previa with anterior implantation, particularly those complicated by placenta accrete syndromes.
- Transverse lie of a large fetus, especially when the membranes are ruptured and the shoulder is impacted in the birth canal.
- Presentation of a fetus in a back-down transverse lie.
- Inadequate space in the poorly developed lower uterine segment for the manipulations required for breech delivery in a small fetus.
- Challenges posed by multiple fetuses, especially if they are malpositioned or preterm.
Peripartum hysterectomy indications
In some instances, and most often because of emergent complications such as intractable hemorrhage, abdominal hysterectomy is indicated following delivery. When performed at the time of cesarean delivery, the operation is termed cesarean hysterectomy. If done within a short time after delivery, it is termed postpartum hysterectomy.
Indications
- Uterine atony
- Abnormal placentation
- Bleeding
- Accrete syndromes
- Uterine extension
- Uterine rupture
- Cervical laceration
- Postpartum uterine infection
- Leiomyoma
- Invasive cervical cancer
- Ovarian neoplasia
Cesarean section-Choice of incision
Vertical vs transverse incision
Transverse incisions follow Langer lines of skin tension, and superior cosmetic results compared with vertical incisions can be achieved. Additionally, decreased rates of postoperative pain, fascial wound dehiscence, and incisional hernia compared with vertical entry are benefits.
Two types of transverse incisions
- Pfannenstiel incision (common): 2-3 cm above the symphysis pubis and slightly curved
- Joel-Cohen incision (Misgav Ladach): 3 cm below the anterior superior iliac spine line and straight
Pfannenstiel incision is selected most frequently for cesarean delivery.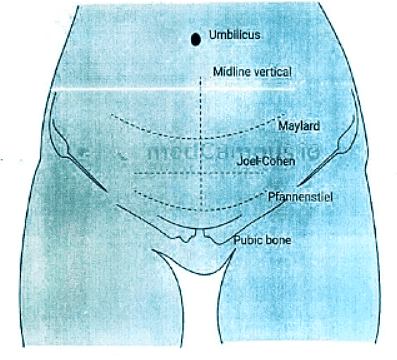
Trial of Labour
- Attempting labor after a previous cesarean, regardless of the outcome of the prior cesarean.
- Vaginal Birth After Cesarean (VBAC): A successful Trial of Labor After Cesarean (TOLAC) resulting in vaginal birth.
Candidate for TOLAC
- One prior low transverse cesarean delivery.
- Clinically adequate pelvis.
- Absence of other uterine scars or previous rupture.
- Access to healthcare facilities equipped for emergencies.
Risk Factors
- Younger age.
- Lack of previous vaginal delivery.
- Induction of labor.
- Fetal weight exceeding 4kg.
Management
- Antenatal counseling on delivery options.
- Early presentation to the obstetric unit during labor.
- Immediate access to cesarean section, blood transfusion services, continuous fetal heart monitoring, specialist obstetricians, anesthetists, and pediatricians around the clock.
- Use of a partogram to track labor progress.
- Administration of epidural analgesia.
- Monitoring for signs of impending scar rupture (incidence 0.5%-1%).
- Signs include abdominal pain, tenderness, pathologic retraction ring, increased uterine irritability, hematuria, and signs of hypovolemic shock.
- Fetal distress during labor is a common sign of scar rupture.
- The second stage of labor should not exceed 2 hours.
Cesarean section-Repeats
Q1: Write down indications of Lower Segment Caesarean Section (L.S.C.S.). How will you suspect the impending scar rupture? What are the advantages of L.S.C.S. over classical Caesarean Section? (2011)
Q2: What is trial of labour? How would you manage a trial of labour in patient who has had a Caesarean Section previously? (2015)
|
7 videos|219 docs
|
FAQs on Cesarean section - Medical Science Optional Notes for UPSC
| 1. What are the common indications for a Cesarean section? |  |
| 2. What are the indications for a peripartum hysterectomy? |  |
| 3. How is the choice of incision made during a Cesarean section? |  |
| 4. What is a trial of labor? |  |
| 5. When is a repeat Cesarean section recommended? |  |

|
Explore Courses for UPSC exam
|

|
















