Ischemic Heart Diseas (IHD) | Medical Science Optional Notes for UPSC PDF Download
| Table of contents |

|
| IHD vs CAD |

|
| Syndromes - IHD |

|
| IHD - Pathogenesis |

|
| IHD - Complication |

|
IHD vs CAD

Syndromes - IHD

Atherosclerosis Risk Factors
Non-modifiable (Constitutional):
- Genetic abnormalities
- Family history
- Advancing age
- Male gender
Modifiable:
- Hyperlipidemia
- Hypertension
- Cigarette smoking
- Diabetes
- Inflammation (CRP levels)
- Hyperhomocysteinemia
- Elevated lipoprotein A levels
- Metabolic syndrome
Plaque Stable vs Unstable


Critical stenosis >70% occlusion
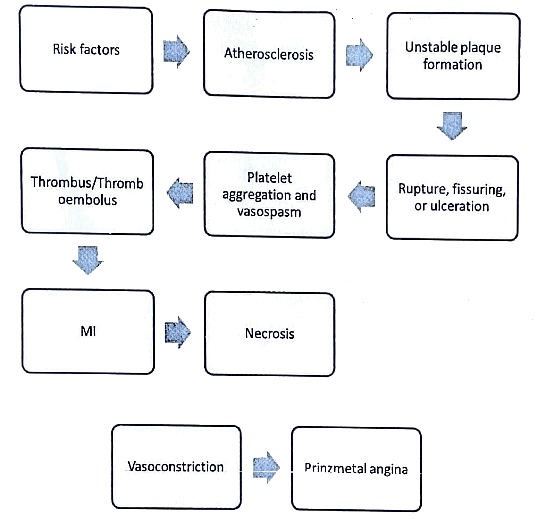
IHD - Pathogenesis
Sequential Myocardial Changes in MI

Lab Investigations in Ml
The laboratory assessment of myocardial infarction (MI) relies on measuring the blood levels of macromolecules that seep out of injured myocardial cells due to damaged cell membranes. These molecules encompass:
- Myoglobin
- Cardiac troponins T and I (TnT, TnI)
- Creatine kinase (CK), specifically the myocardial isoform, CK-MB
- Lactate dehydrogenase


IHD - Complication
- Rupture of the myocardium
- Impaired contractile function
- Development of arrhythmias
- Onset of pericarditis
- Formation of ventricular aneurysm
- Dilatation of cardiac chambers leading to progressive late-stage heart failure (chronic IHD)
- Infarct expansion associated with mural thrombus
- Dysfunction of papillary muscles
- Involvement of the right ventricle

In general, individuals experiencing anterior infarcts tend to have a more unfavorable clinical prognosis compared to those with posterior infarcts.
IHD - Repeats
- Discuss pathogenesis and pathology of ischemic heart disease (1999)
- Give the morphological changes and complications in myocardial infarction (2007).
- What are sequential myocardial changes in myocardial infarction?
Discuss the laboratory investigations in a case of myocardial infarction. (2016)
|
7 videos|219 docs
|
FAQs on Ischemic Heart Diseas (IHD) - Medical Science Optional Notes for UPSC
| 1. What is the difference between IHD and CAD? |  |
| 2. What are the common syndromes associated with IHD? |  |
| 3. What is the pathogenesis of IHD? |  |
| 4. What are the complications of IHD? |  |
| 5. How is IHD diagnosed and treated? |  |

|
Explore Courses for UPSC exam
|

|