Neglected Areas in Health—An Indian Scenario | UPSC Mains Essay Preparation PDF Download
Structure
(1) Opening
- Communicable diseases are growing in both developed and developing countries.
(2) Body
- The ageing of the population brings to us the most costly non-communicable diseases.
- Misallocation of public money to more curative and low-cost-effective interventions required special attention.
- Sixty per cent of the health budget is utilised in urban areas.
- Need for effective and acceptable prophylactic vaccination against rabies.
- In health planning and budgeting mental disorders have received a very low priority
- Developing countries should be self-sufficient in producing vaccines.
(3) Closing
- Health for all - Investment
Model Essay
The global health landscape has evolved significantly in recent decades, with the developed world largely overcoming most communicable diseases. However, the battle against such diseases continues in many developing countries, which remain vulnerable due to inadequate healthcare infrastructure and limited access to vaccines and medicines. At the same time, non-communicable diseases (NCDs), including heart disease, cancer, and diabetes, have emerged as major public health threats in both developed and developing nations. According to the World Health Organization (WHO), NCDs now account for over 70% of global deaths, making them a top priority for healthcare systems worldwide.
In India, the healthcare system faces a myriad of challenges. While progress has been made in eradicating diseases such as smallpox and polio, the country is still struggling with both infectious diseases and the rise of chronic conditions, which have increased the burden on an already strained healthcare system. The WHO has stated that “the shift from communicable to non-communicable diseases is a sign of a nation’s development, but it also represents the growing burden on health systems” (WHO, 2018). In India, this shift is particularly concerning due to the country’s rapid urbanization and adoption of unhealthy lifestyle habits. Smoking, poor dietary patterns, and lack of physical activity are major contributors to the rising rates of NCDs.
India’s healthcare is a state subject, meaning that it is primarily the responsibility of state governments to provide healthcare services. However, this has resulted in regional disparities, with urban areas receiving the majority of resources despite housing only a small fraction of the population. According to a report by the National Commission on Macroeconomics and Health (NCMH), “approximately 60% of health expenditure in India is concentrated in urban areas, even though 70% of the population resides in rural areas.” This inequitable distribution of healthcare resources leaves rural populations, where health infrastructure is weakest, vulnerable to both communicable and non-communicable diseases.
Public health interventions have been responsible for significant progress, such as the eradication of smallpox and the reduction of childhood mortality rates through vaccination programs. However, the burden of diseases like rabies, tuberculosis, and malaria persists in India. Rabies, for example, causes approximately 20,000 deaths annually, and the WHO estimates that “80% of rabies deaths occur in rural areas, where access to post-exposure prophylaxis is limited.” Despite this, India has made strides in addressing these diseases, with initiatives like the National Rabies Control Program aimed at reducing the incidence of rabies through better vaccination coverage and awareness.
Non-communicable diseases, including cardiovascular diseases, diabetes, and respiratory disorders, are now among the leading causes of death in India. WHO’s Director-General, Dr. Tedros Adhanom Ghebreyesus, has emphasized that “tobacco use is the leading preventable cause of death globally, and its control is a priority for global health.” India’s tobacco use, which affects a significant portion of the adult population, continues to be a major public health issue that demands urgent attention.
Mental health is another area that has been largely neglected in India’s healthcare planning. Around 10-15% of India’s population suffers from psycho-social problems, and about 1-2% from severe mental disorders. Despite the high prevalence, mental health services remain underfunded and poorly integrated into the healthcare system. India’s National Mental Health Policy, adopted in 2014, has made some strides, but there is still a long way to go in terms of funding, infrastructure, and public awareness.
The agricultural sector, which employs a significant portion of India’s rural population, also presents a unique set of health challenges. Farmers are frequently exposed to hazardous chemicals such as pesticides and fertilizers, leading to a higher incidence of occupational diseases. A report by the Food Safety Department (WHO) states, “pesticide exposure is a serious concern for agricultural workers, leading to long-term health complications.” Poor healthcare facilities, inadequate nutrition, and vulnerability to natural disasters further exacerbate the health risks faced by rural communities.
To address these challenges, India must invest in improving its healthcare infrastructure, particularly in rural areas. Additionally, it should focus on enhancing preventive healthcare measures, such as vaccination programs and awareness campaigns about the dangers of tobacco use and poor diet. Self-sufficiency in vaccine production, which would reduce reliance on imports, is another crucial step toward improving India’s healthcare outcomes.
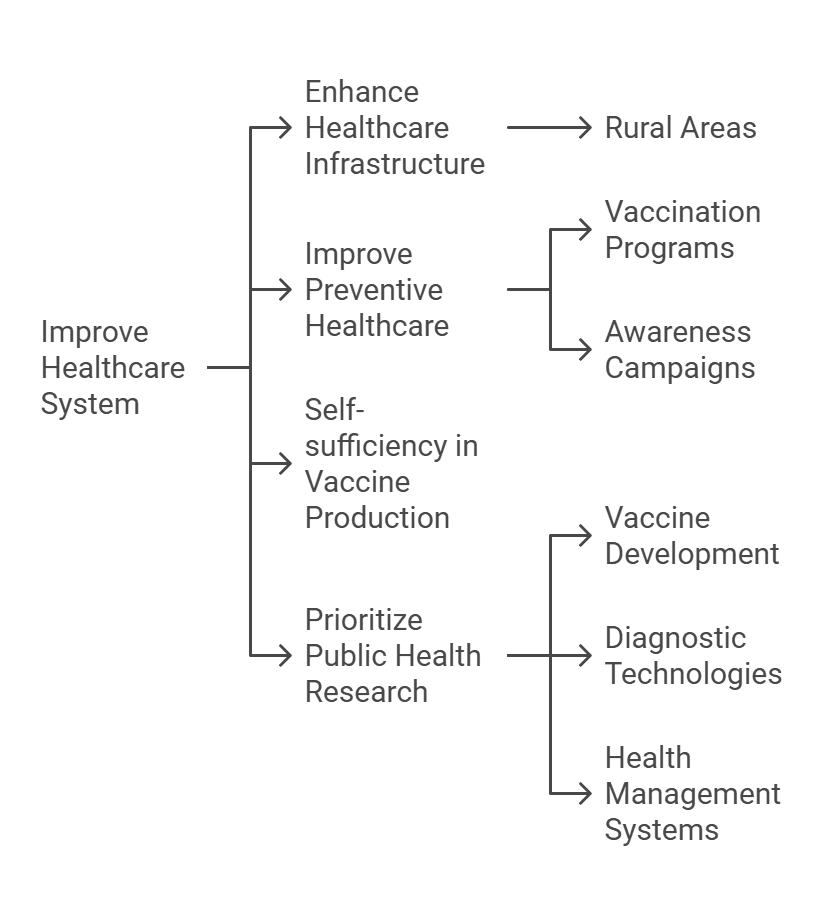
Furthermore, India should prioritize research in public health, particularly in areas such as vaccine development, diagnostic technologies, and health management systems. Space technology, including remote sensing, has shown promise in monitoring environmental factors that affect public health, such as air pollution and waterborne diseases. The use of biosensors and other advanced technologies for disease monitoring is an area of growing interest that could help improve public health surveillance and response capabilities.
In conclusion, India faces a complex array of public health challenges, from the continued threat of infectious diseases to the rising burden of non-communicable diseases. The country must adopt a multi-pronged approach to address these issues, focusing on equitable resource distribution, strengthening preventive healthcare, and investing in research and technological innovation. As the WHO rightly states, “the health of a nation is its greatest asset.” By improving healthcare infrastructure, addressing social determinants of health, and ensuring access to quality services for all citizens, India can pave the way for a healthier future for its population.
|
4 videos|178 docs
|
FAQs on Neglected Areas in Health—An Indian Scenario - UPSC Mains Essay Preparation
| 1. What are the major neglected health issues in India today? |  |
| 2. How does socioeconomic status affect health in neglected areas of India? |  |
| 3. What role does government policy play in addressing neglected health issues in India? |  |
| 4. How can community involvement improve health in neglected areas of India? |  |
| 5. What are some successful interventions to tackle neglected health issues in India? |  |





















