Organ Function Tests | Medical Science Optional Notes for UPSC PDF Download
| Table of contents |

|
| Kidney/Renal Function Tests |

|
| Liver Function Tests |

|
| Types of Jaundice |

|
| Thyroid Function Tests |

|
Organ function tests, which offer insights into the performance of specific organs, are commonly categorized as tests assessing the functionality of organs. These comprehensive tests encompass evaluations of kidney, liver, and thyroid function.
Kidney/Renal Function Tests
The kidneys, crucial organs in the body, carry out essential functions, including:
- Maintenance of homeostasis
- Excretion of metabolic waste products
- Retention of substances vital to the body
- Hormonal functions
Notable hormones produced by the kidneys include Erythropoietin, 1,25-Dihydroxycholecalciferol (calcitriol), and Renin.
The renal threshold of a substance is defined as its concentration in the blood (or plasma) beyond which it is excreted into urine. The renal thresholds for specific substances are as follows: glucose (180 mg/dl), ketone bodies (3 mg/dl), calcium (10 mg/dl), and bicarbonate (30 mEq/l).
The term "tubular maximum" (Tm) is employed to express the maximum capacity of the kidneys to absorb a particular substance. For example, the tubular maximum for glucose (TmG) is 350 mg/min.
A Complete Urinalysis
Encompassing the evaluation of urine's physical and chemical attributes, the assessment involves the following:
Physical characteristics under scrutiny comprise:
- Urine volume (typically requiring a timed urine sample, often over 24 hours)
- Odor
- Color
- Appearance (clear or turbid)
- Specific gravity
- pH
Chemical characteristics involve the identification of abnormal constituents in urine associated with various disease conditions, such as:
- Protein (linked to Nephrotic syndrome and Diabetic nephropathy)
- Glucose (associated with Diabetes Mellitus)
- Blood (indicative of Glomerulonephritis, UTI, and Renal cell carcinoma)
- Ketone bodies (connected to Diabetic ketoacidosis and Starvation)
- Bile salts and bile pigments (related to Liver disease)
- Urea and Creatinine
Proteinuria/Albuminuria
Under normal circumstances, the excretion of protein in urine is typically less than 150 mg, and the excretion of albumin is usually less than 30 mg within a 24-hour period. These levels fall below the detection limit of routine tests. Exceeding these thresholds is termed proteinuria, indicating the presence of renal disease. The primary cause of proteinuria often involves the compromised integrity of the glomerular basement membrane, a condition known as glomerular proteinuria, commonly observed in nephrotic syndrome and diabetic nephropathy.
In cases of glomerular proteinuria, the predominant protein is albumin. Microalbuminuria is defined as the presence of 30 to 300 mg of albumin in a 24-hour urine sample and serves as an early marker for renal damage in diabetes mellitus.
Urea and creatinine are substances excreted in urine, and their concentrations in the serum can function as markers for renal function. This is because their serum concentrations tend to increase as renal function declines.
Creatinine serves as a superior indicator of renal function compared to urea, as its blood concentration remains relatively unaffected by non-renal factors, rendering it a specific marker for renal function. Conversely, various factors can influence blood urea concentration.
While serum creatinine serves as a marker for renal function, a substantial increase in blood concentration is evident only when there is approximately a 50% decline in the glomerular filtration rate (GFR). Consequently, the measurement of serum creatinine is a test with limited sensitivity. Creatinine clearance measurement provides an estimate of GFR, allowing for the detection of early stages of renal failure.
The quantity of creatinine excreted is proportionate to the total creatine phosphate content in the body and, consequently, muscle mass. Typically, the daily excretion of creatinine remains relatively constant.
Serum creatinine concentration remains unaffected by both endogenous and exogenous factors, in contrast to urea, which can be influenced by various factors. The intake of a protein-rich meal, for instance, increases the level of N-acetylglutamate in the liver, leading to enhanced urea production. Additional factors affecting blood urea levels include certain medications such as steroids and antibiotics (resulting in increased or decreased BUN levels), pregnancy, and the aging process.
For this reason, some experts regard serum creatinine as a more dependable indicator of renal function. Clearance, in the context of renal function, refers to the volume of plasma from which a compound is entirely cleared by the kidneys in a given unit of time. This can be calculated using the formula: Clearance (mL/min) = (U x V)/P, where U represents the concentration of the measured analyte in a timed urine sample (typically over 24 hours), P is the plasma concentration of the analyte, and V is the volume of urine produced per minute.
A substance suitable for measuring renal clearance possesses characteristics such as a relatively stable blood concentration, exclusive excretion through urine, free filtration at the glomerulus, and absence of reabsorption or secretion by the renal tubules.
While creatinine clearance is a frequently used measure, it tends to overestimate glomerular filtration rate (GFR) due to its slight secretion by the renal tubules. Inulin clearance, on the other hand, meets all the criteria necessary for a compound used in clearance tests. However, unlike creatinine, inulin is an exogenous substance that requires intravenous infusion at a constant rate.
Other compounds which help in calculation of Clearance are Urea clearance test (values are slightly lower than usual GFR due to partial reabsorption by the tubules), 51Cr EDTA.
Clearance of PAH (Para Amino Hippuric acid) represents the renal plasma flow

Production and metabolism of Bilirubin

Liver Function Tests
Functions of liver
- Metabolism Intermediary
- Protein Metabolism
(a) Deamination of amino acids
(b) Urea Formation (Krebs-Henseleit cycle), facilitating the removal of toxic ammonia
(c) Formation of plasma proteins - Carbohydrate Metabolism
(a) Regulation of glycogen metabolism - Lipid Metabolism
(a) Hepatocellular uptake and metabolism of lipoproteins
(b) Lipogenesis
- Protein Metabolism
- Synthesis of Coagulation Factors
- Embryonic Erythropoiesis
- Bilirubin Metabolism
- Endocrine Functions (Angiotensinogen/Thrombopoietin/IGF-1)
- Immune Functions - Involvement of Kupffer cells
- Metabolism and Excretion of Drugs
- Storage Functions - Vitamin A, D, B12, Glycogen, Trace Element Iron

Biochemical Evaluation of Jaundice
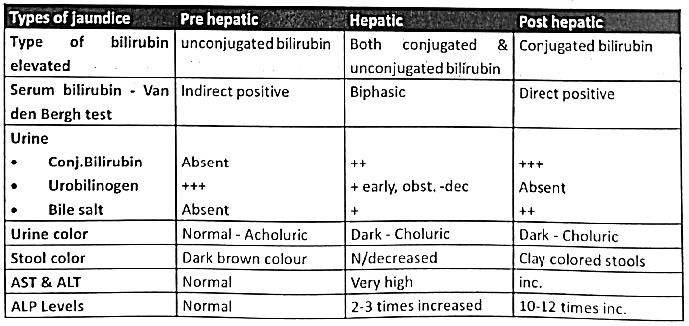
The typical range for normal serum total bilirubin concentration is 0.2 to 1.0 mg/dl. Jaundice is a clinical condition identified by a yellow discoloration of the sclera and skin, resulting from the accumulation of bilirubin due to elevated levels in the serum. Jaundice is categorized into three primary types: hemolytic, hepatic, and obstructive.
Hemolytic Jaundice:
This condition is linked to an increased breakdown of erythrocytes, leading to the excessive production of bilirubin that surpasses the liver's capacity for conjugation and excretion. Hemolytic jaundice is characterized by:
- Elevation of serum unconjugated bilirubin
- Increased excretion of urobilinogen in urine
- Dark brown color of feces due to a high content of urobilinogen
Hepatic (Hepatocellular) Jaundice:
This form of jaundice arises from liver dysfunction resulting from damage to parenchymal cells. Liver damage impairs bilirubin uptake and its conjugation by liver cells. Causes include:
- Viral infections (viral hepatitis)
- Exposure to poisons and toxins (chloroform, carbon tetrachloride, phosphorus, etc.)
- Cirrhosis of the liver
- Cardiac failure
Hepatic jaundice is characterized by:
- Elevated levels of both conjugated and unconjugated bilirubin in the serum
- Dark-colored urine due to excessive bilirubin excretion
- Passage of pale, clay-colored stools due to the absence of urobilinogen
- Increased activity of alanine transaminase (SGPT) and aspartate transaminase (SGOT) released into circulation as a result of hepatocyte damage.
This results from a blockage in the bile duct, hindering the flow of bile into the intestine. Potential causes of this obstruction may include gallstones, tumors, and other factors. The blockage in the bile duct causes the release of conjugated bilirubin from the liver into the circulation.
Obstructive jaundice is identified by:
- An elevated concentration of conjugated bilirubin in the serum.
- Elevated serum alkaline phosphatase, released from damaged bile duct cells.
- Dark-colored urine resulting from increased bilirubin excretion.
- Pale, clay-colored feces due to the absence of urobilinogen.
Van den Bergh Reaction
Van den Bergh reaction is highly useful in understanding the nature of jaundice.
Principle:
Diazotized sulfanilic acid swiftly produces a purple color when it reacts with conjugated bilirubin—this is known as the Direct Positive Van den Bergh Reaction. This color change occurs immediately, typically within 30 seconds.
When diazotized sulfanilic acid, combined with methanol (a dissolving agent), reacts with unconjugated bilirubin, a purple color typically develops within 30 minutes. This variation is referred to as the Indirect Positive Van den Bergh Reaction.
In cases where the serum contains elevated concentrations of both unconjugated and conjugated bilirubin, the purple color appears promptly. The addition of alcohol further intensifies this coloration, resulting in what is known as the Biphasic Van den Bergh Reaction.
Types of Jaundice
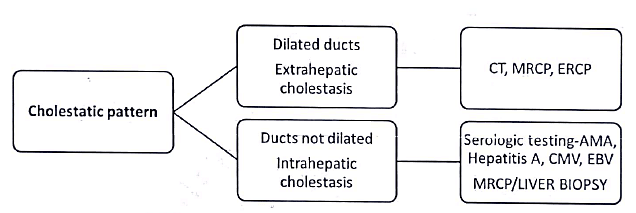
Management Algorithm for Patient with Jaundice



Liver function Tests-Repeats
Liver:
- Elaborate on the significance of enzyme assays in evaluating liver function (2010).
- Define jaundice and provide a concise overview of the formation and destiny of bilirubin. Highlight the major distinctions among the three types of jaundice (2011).
- Discuss tests based on the intermediary metabolic functions of the liver, elucidating the underlying principles of each test (2011).
- Define obstructive jaundice and outline the diverse biochemical tests recommended for the patient. Explain the biochemical rationale for the anticipated changes (2014).
- Create a table outlining the results of various biochemical tests in the blood and urine of patients with pre-hepatic, hepatic, and post-hepatic jaundice (2017).
Thyroid Function Tests



Functions of TSH:
- Facilitates the uptake of iodide (iodide pump) from the bloodstream by the thyroid gland.
- Augments the conversion of iodide (I-) to active iodide (I*), a process referred to as organification.
- Elevates the proteolysis of thyroglobulin, releasing T3 and T4 into the circulation.
- Amplifies the synthesis of proteins, nucleic acids, and phospholipids in the thyroid gland.
Biochemical Roles of Thyroid Hormones
Triiodothyronine (T3) exhibits approximately four times greater biological activity than thyroxine (T4).
- Impact on Metabolic Rate: Thyroid hormones stimulate metabolic activities, leading to increased oxygen consumption in most body tissues (with exceptions such as the brain, lungs, testes, and retina).
- Influence on Protein Synthesis: Functioning akin to steroid hormones, thyroid hormones promote protein synthesis. They operate as anabolic hormones, fostering a positive nitrogen balance and supporting growth and development.
- Effects on Carbohydrate Metabolism: Thyroid hormones facilitate the intestinal absorption and utilization of glucose. They also enhance gluconeogenesis and glycogenolysis, collectively elevating blood glucose levels (resulting in hyperglycemia).
- Impact on Lipid Metabolism: Thyroid hormones stimulate lipid turnover and utilization. Hypothyroidism is associated with elevated plasma cholesterol levels, a condition that can be reversed through the administration of thyroid hormones.
The thyroid's parafollicular C cells originate from a neuroendocrine source and migrate to the thyroid through the ultimobranchial body. These cells are responsible for producing calcitonin.
Calcitonin plays a role in the regulation of calcium and phosphate levels in the bloodstream, acting in opposition to the effects of parathyroid hormone.
Results of thyroid function tests in normal and pathological states.

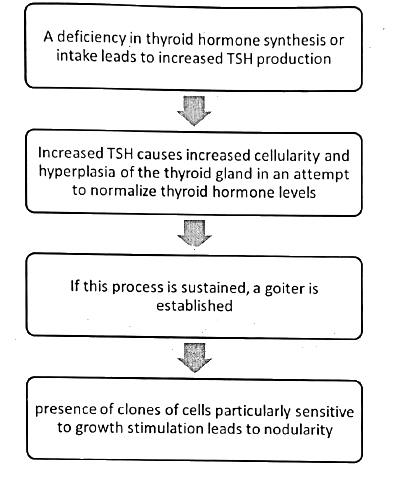
Evaluation of Goitre
Any abnormal increase in the size of the thyroid gland is known as goiter

Repetitive Organ Function Tests
Thyroid Gland
- List the hormones released by the thyroid gland. Explain the mechanism behind thyroid enlargement in cases of iodine deficiency in the diet (2003).
- The occurrence of nodular growth in the neck is prevalent among populations residing in mountainous regions. What are the reasons for this phenomenon, and how would you go about investigating such cases? (2012)
- Outline the thyroid function tests. Provide the biochemical observations associated with hyperthyroidism and hypothyroidism (2016).
|
7 videos|219 docs
|
FAQs on Organ Function Tests - Medical Science Optional Notes for UPSC
| 1. What are kidney/renal function tests? |  |
| 2. Why are liver function tests important? |  |
| 3. What are the different types of jaundice? |  |
| 4. What are thyroid function tests? |  |
| 5. What are organ function tests and why are they important? |  |

|
Explore Courses for UPSC exam
|

|

















