Pleural effusion | Medical Science Optional Notes for UPSC PDF Download
Pleural effusion-Etiology
Pleural effusion refers to the buildup of fluid in the pleural cavity, located between the lung lining (visceral and parietal pleurae) and the thoracic cavity. The fluid in the pleural cavity is termed a transudate when it filters through the walls of largely intact pulmonary vessels. In contrast, it is labeled an exudate when it leaks into the pleural cavity due to damage or lesions in blood and lymph vessels, often resulting from inflammation or tumors.

Clinical presentation
- Pleural effusion becomes noticeable when it exceeds 300 mL.
- Manifestations include pleuritic chest pain, a dry, nonproductive cough, and dyspnea.
- Additional symptoms may indicate the underlying disease, such as fever in empyema or cachexia in cases of malignancy. Symptoms of left-sided heart failure may also be present.
Diagnosis
Percussion over the affected area produces a dull tone, and auscultation reveals diminished or entirely absent breath sounds.
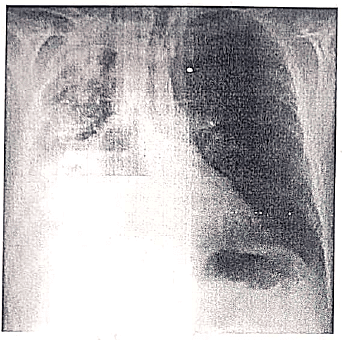
Chest X Ray
- The earliest sign of pleural effusion on a frontal view is the blunting of the lateral costophrenic angle.
- Blunting becomes evident with a minimal fluid amount of approximately 175 mL.
- Chest ultrasound is valuable for assessing suspected pleural effusions and guiding thoracentesis procedures.

Thoracentesis
- Typically, the thoracentesis needle is inserted in the posterolateral aspect of the back, positioned beneath the fluid level but over the diaphragm.
- The insertion is made over the top (superior margin) of the rib to steer clear of intercostal nerves and blood vessels running beneath the rib's underside (near the inferior margin).
- It is essential to conduct a chest X-ray post-procedure to exclude the possibility of a pneumothorax.
Lights criteria
Exudative pleural effusions satisfy at least one of the following criteria, while transudative pleural effusions fulfill none:
- Pleural fluid protein to serum protein ratio exceeding 0.5.
- Pleural fluid LDH to serum LDH ratio surpassing 0.6.
- Pleural fluid LDH exceeding two-thirds of the normal upper limit for serum.


Pleural effusion-Management
Treat the underlying cause (e.g., loop diuretics for acute left heart failure, antibiotics for pneumonia, anti-tuberculous therapy for tuberculosis).
- Symptomatic treatment:
- Tube thoracostomy: Used in recurrent or urgently draining infected/loculated effusions.
- Video-assisted thoracoscopic surgery (VATS): Indicated for histological sampling in malignant effusions, parapneumonic effusions not sufficiently controlled by drainage, and pleural empyema.
- Pleurodesis:
- Indication: Malignant effusions or effusions not responding to drugs (e.g., diuretics, antibiotics).
- Technique: Chemical or surgical pleurodesis.
- Patients with recurrent chylothorax or recurrent malignant effusions may require pleuroperitoneal shunts.
Empyema
- Definition: Accumulation of pus in the pleural cavity.
- Etiology: Most commonly results from an infected parapneumonic pleural effusion. Less common causes include untreated hemothorax, ruptured lung abscess, esophageal tear, or thoracic trauma (e.g., thoracic surgery).
- Clinical Features:
- Pleuritic chest pain
- Shortness of breath
- Low-grade fever
- Cough
- Diagnosis:
- Chest X-ray: May resemble pleural effusion with blunting of the costophrenic angle; often loculated. Large empyema can show diffuse lung consolidation.
- Chest CT: Effective in differentiating empyema from pleural effusion. Unilateral and asymmetric appearance. Features like the split pleura sign, thickening of visceral and parietal pleura due to fibrin adherence, and septations.
- Thoracocentesis: Pleural fluid analysis revealing low glucose (<60 mg/dL) and pH < 7.2, indicating empyema. Refer to distinguishing features of exudate.

- Treatment:
- Utilize a chest tube (thoracostomy) to evacuate empyema fluid.
- Consider intrapleural administration of fibrinolytic agents to enhance chest tube drainage of empyema fluid.
- If empyema persists despite chest tube drainage, opt for thoracoscopic debridement, involving the removal of pus and pleural fibrosis.
- Administer systemic antibiotics based on culture and sensitivity testing for appropriate treatment.
Pleural effusion-Repeats
Q1: What is empyema? Discuss the management of a case with empyema. (2012)
Q2: A 35 years old patient comes with chest pain on left side. There is also history of high-grade fever for the last 3 days. Write your differential diagnosis. How will you manage a case of acute pneumonitis? (2007)
Q3: A 40-year-old Non-Resident Indian visiting India develops acute, sudden breathlessness one week after landing in India. A resident of USA, he has no such previous history of breathlessness. (2015)
(i) List the differential diagnosis.
(ii) How would you investigate this patient?
|
7 videos|219 docs
|
FAQs on Pleural effusion - Medical Science Optional Notes for UPSC
| 1. What is the main cause of pleural effusion? |  |
| 2. How is pleural effusion managed? |  |
| 3. Can pleural effusion recur? |  |
| 4. What are the symptoms of pleural effusion? |  |
| 5. Is pleural effusion a life-threatening condition? |  |

|
Explore Courses for UPSC exam
|

|