NEET Exam > NEET Notes > Key Notes: Breathing & Exchange of Gases
Key Notes: Breathing & Exchange of Gases - NEET PDF Download
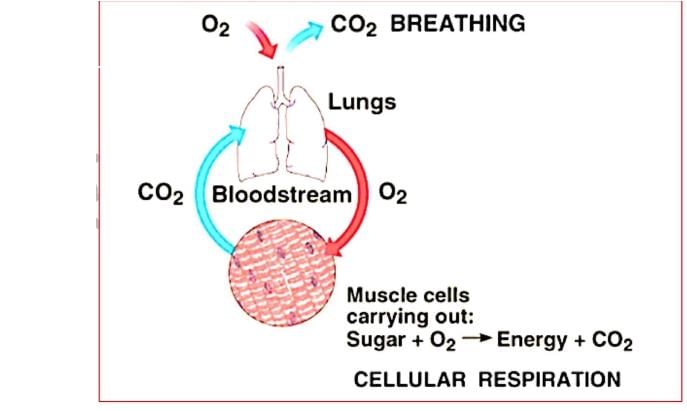
- Breathing → Process of exchange of O2 from the atmosphere with CO2 produced by the cells is called breathing, commonly known as respiration.
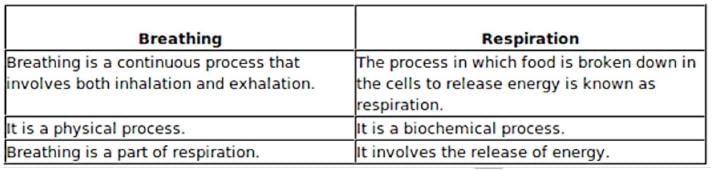
- Respiration takes place in three steps - Pulmonary ventilation - It is exchange of air between atmosphere and lungs.
- External/Pulmonary Respiration - It is exchange of gases between air space in lungs and blood in pulmonary capillary.
- Internal/Tissue Respiration - Exchange of gases between blood in systemic capillary and tissue cells. In this process blood loses O2 and receive CO2 from tissue.
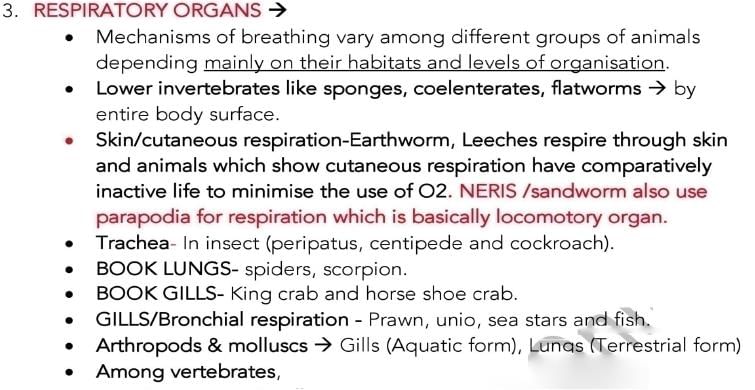
- Respiratory medium in environment is either air (for terrestrial organisms) or water for aquatic organism.

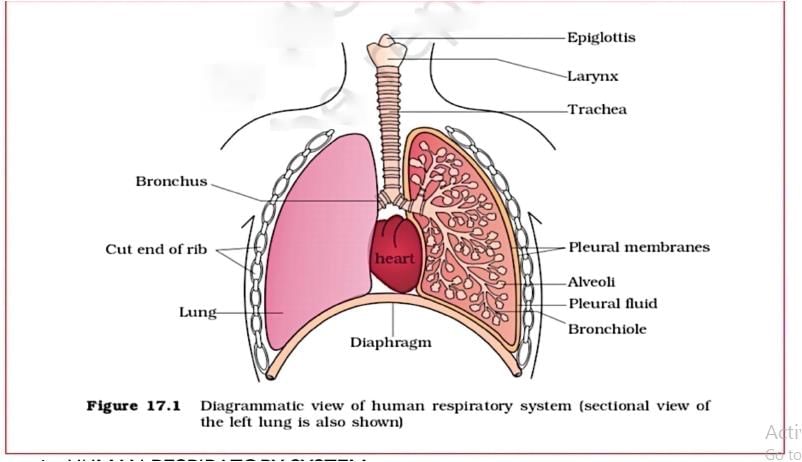
- Opening by which pharynx open into larynx/voice box is called glottis and it generally remain open but during swallowing it is closed by thin elastic cartilaginous epiglottis.
- Epiglottis prevent the entry of food in trachea.
- Opening of pharynx into oesophagus is through aperture called gullet and it generally remain closed and become open during swallowing.
- Larynx is a cartilaginous box which helps in sound production and hence called the sound box.
- Trachea is a straight tube of about 12 cm in length and 2.5 cm in diameter extending up to the mid-thoracic cavity, which divides at the level of 5th thoracic vertebra into a right and left primary bronchi.
- Trachea wall consist of fibre, cartilage and muscles and mucous membrane.
- Division of trachea take place in this order:
Trachea → Pair of primary bronchi → secondary bronchi Tertiary bronchi/segmental bronchi Terminal bronchiole → respiratory bronchiole alveolar duct - atrium alveolar sac alveoli/air sac.
- As we go down from trachea to downside diameter decreases.
- Alveoli is thin, irregular walled and vascularised bag.
- From trachea to terminal bronchiole it is called dead space /conducting passage. It also includes nose area. There is no exchange of gases.
- From respiratory bronchiole to alveoli, it is called respiratory zones where gaseous exchange takes place.
- The tracheae, primary, secondary and tertiary bronchi, and initial bronchioles are supported by Incomplete Cartilaginous Rings.
- The branching network of bronchi, bronchioles and alveoli comprise the lungs.
Human Lungs
- Two lungs
- Covered by a double layered Pleura.
- Between layers of pleura with Pleural Fluid present.
- Pleural fluid reduces friction on the lung-surface.
- Plural fluid is glycoprotein in nature and secreted by pleura. Pressure inside plural cavity is - 5mm Hg.
- The outer pleural membrane → close contact with the thoracic lining whereas Inner pleural membrane.→. if contact with the lung surface.
- The conducting part transports the atmospheric air to the veoli, clears it from foreign articles, humidifies and also brings the air to body temperature.
- Exchange part is the site of actual diffusion of O2 and CO2 between blood and atmospheric air.
- The lungs are situated in the Thoracic chamber which is anatomically an air-tight chamber.
- The Thoracic chamber is formed:
1. dorsally by the vertebral column
2. ventrally by the sternum
3. laterally by the ribs
4. on the lower side by the dome-shaped diaphragm. - The anatomical setup of lungs in thorax is such that any change in the volume of the thoracic cavity will be reflected in the lung (pulmonary) cavity.
- Such an arrangement is essential for breathing
Steps of Respiration:
- Breathing or pulmonary ventilation
- Atmospheric air intake and CO2 rich alveolar air is released.
- Diffusion of gases across alveolar membrane.
- Transport of gases by the blood.
- Diffusion of O2 and CO2 between blood and tissue.
- Utilisation of O2 by the cells (cellular respiration)
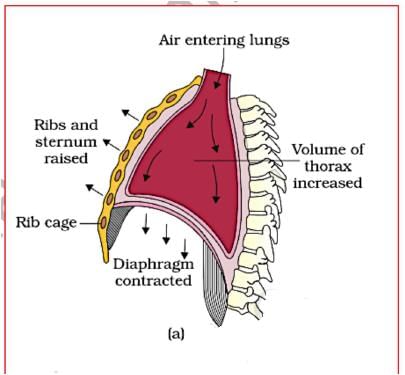
Mechanism of Breathing
- Breathing involves two stages :
1) Inspiration during which atmospheric air is drawn in.
2) Expiration by which the alveolar air is released out. - The movement of air into and out of the lungs is carried out by creating a pressure gradient between the lungs and the atmosphere.
- Inspiration can occur ⇒ If the pressure within the lungs (intra-pulmonary pressure) is less than the atmospheric pressure and it is Active process.
- Expiration takes place When the intra-pulmonary pressure is higher than the atmospheric pressure. Normal expation is passive process.
How Pressure Changes
- The diaphragm and a specialised set of muscles - external and internal intercostals between the ribs, help in generation of such gradients.
- Inspiration is initiated by
- The contraction of diaphragm → increases the volume of thoracic chamber in the antero-posterior axis.
- Diaphragm is principle muscles of inspiration.
- It is skeletal muscle attach to the sternum.vertebral column and rib and formed of radial muscles fiber.
- In relaxed state, it is dome shape and convex towards thoracic cavity concave towards the abdominal cavity.
- During inspiration diaphragm it contract (active process) become straight and descend down which increase thorasic cavity.
- Phrenic nerve is present in diaphragm.
- If diaphragm punctured, respiration will stop and patient will die.
- In full term pregnancy contribution of diaphragm is 0%.
- The contraction of external inter-costal muscles lifts up the ribs and the sternum → an increase in the volume of the thoracic chamber in the dorso-ventral/anteroposterior axis.
- Whereas diaphragm contraction causes increase in vertipaf-’ diameter of thorasic cavity → The overall increase in the thoracic volume → causes a similar increase in pulmonary volume.
- An increase in pulmonary volume
- Decreases the intra-pulmonary pressure (to less than the atmospheric pressure).
- This decreased pressure forces the air from outside to move into the lungs, i.e.. inspiration.
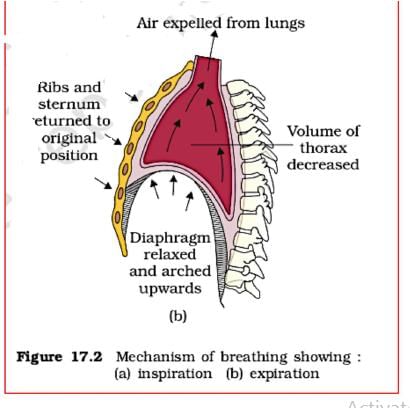
- Expiration is initiated by: Relaxation of the diaphragm and the external inter-costal muscles returns the diaphragm and sternum to their normal positions therefore ribs move inferiorly and diaphragm become dome shape again and Reduce the thoracic volume and thereby the pulmonary volume.
- This leads to an increase in intra-pulmonary pressure to slightly above the atmospheric pressure causing the expulsion of air from the lungs, i.e.. expiration.
- Normal expiration is passive process but forced expiration is Active process in which internal costal muscles and abdominal muscles take part and reduce the thorasic volume.
- Role of Abdominal Muscles: 4 Ability to increase the strength of inspiration and expiration.
- Respiration rate → A healthy human breathes 12-16 times/minute.
- Spirometer Apparatus: used to measure volume of air involved in breathing movements which helps in clinical assessment of pulmonary functions.
Respiratory Volumes and Capacities
- Tidal Volume (TV):
1. Volume of air inspired or expired during a normal respiration.
2. It is approx. 500 mL - Inspiratory Reserve Volume (IRV):
1. Additional volume of air, inspire by a forcible inspiration.
2. 2500 mL to 3000 mL. - Expiratory Reserve Volume (ERV):
1. Additional volume of air, expire by a forcible expiration.
2. 1000 mL to 1100 mL. - Residual Volume (RV):
1. Volume of air remaining in the lungs even after a forcible expiration.
2. 1100 mLto 1200 mL. - Inspiratory Capacity (IC)
IC = TV + IRV (500+3000= 3500)ml - Expiratory Capacity (EC)
EC = TV+ERV (500+1100=1600)ml - Functional Residual Capacity (FRC)
FRC = ERV+RV (1100+1200=2300)ml - Vital Capacity (VC)
VC = ERV+TV+IRV (1100+500+3000=4600)ml - Total Lung Capacity(TLC)
TLC = RV+ERV+TV+IRV or VC + RV (4600+1200=5800)ml - Total volume of air accommodated in the lungs at the end of a forced inspiration.
- Vital capacity+ residual volume
TV=500ml. rRV=3000ml. ERV=1100ml RV= 1200ml.
IC=3500ml.
EC=1600ml.
ZASFRC=2300ml.
VC=4600ml.
TLC=5800ml.
Note: Residual volume can not be measured in spirometer as it is present indead space.
Exchange of Gases
- Alveoli are the primary sites of exchange of gases.
- Exchange of gases also occur between blood and tis
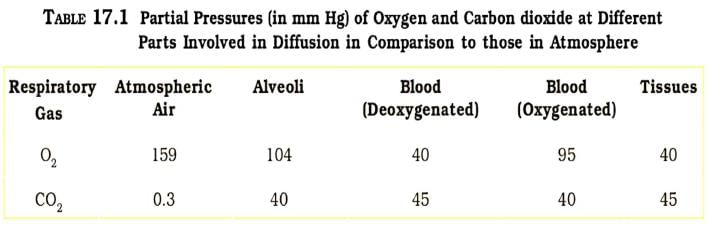
- O2 and CO2 are exchanged in these sites by sir based on pressure/concentration gradient.
- Important factors that can affect the rate of diffusion.
- Solubility of the gases.
- The thickness of the membranes involved in diffusion.
- Partial pressure → Pressure contributed by an individual gas in a mixture of PO2 for oxygen and PCO2 for carbon dioxide.Partial pressure of O2 in atmosphere is 159mm.
- Only about 0.3ml 02(1,5%of 02) is dissolve in blood plasma and 19.7ml of O2(98.5%of 02) is carried by RBC in 100ml of blood. Pressure of O2 is highest in inspired air (158) and jest in lowest in tissue cells (20-40mrm) and it is opposite for CO2 that in inspired air it is 0.3mm and in tissue cell 45-52mm.
- Diffusion Direction:
- A concentration gradient for oxygen from alveoli to blood and blood to tissues.
- A gradient is present for CO2 in the opposite direction, i.e., from tissues to blood and blood to alveoli.
- As the solubility of CO2 is 20-25 times higher than that of O2, So the amount of CO2 that can diffuse through the diffusion membrane per unit difference in partial pressure is much higher compared to that of O2 .
- Blood reaching to tissue capillaries has always higher PO2 than that of tissue cell as tissue cell use O2 for oxidation process and tissue cells also has higher PCO2 than tissue capillary as it is by-product of cellular respiration and these differences is the reason of diffusion of gases at this place.
- Exchange of gases in the tissue lower the PO2 of blood and raise the PCO2 of blood → internal respiration. And this venous blood (High PCO2 )is send to right atrium then to lungs for oxygenation.
- The diffusion membrane/Alveolocapillary membrane /respiratory membrane made up of three major layers:
a. the thin squamous epithelium of alveoli,
b. the endothelium of alveolar capillaries and
c. the basement substance in between them. - Total thickness less than a millimetre. (0.5micrometer)
Transport of Gases
- Blood is the medium of transport for O2 and CO2 .
- Oxygen Transport: 97% by RBCs in the blood and 3 % in a dissolved state through the plasma.
- CO2 Transport: 20-25% by RBCs, 70% as bicarbonate in plasma and 7% dissolved state through plasma.
- Haemoglobin is a red coloured iron containing pigment present in the RBCs. O2 can bind with haemoglobin in a reversible manner to form oxyhaemoglobin. Each haemoglobin molecule can carry a maximum of four molecules of O2 . Binding of oxygen with JHp is primarily related to partial pressure of O2. Partial pressure of CO2 , hydrogen ion concentration and temperature → can interfere with oxygen binding.
- A sigmoid curve is obtained when percentage saturation of haemoglobin with O2 is plotted against the PO2:
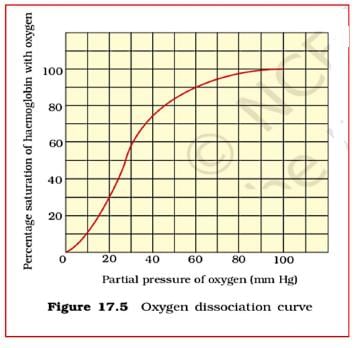
Oxygen-Hb Dissociation Curve
- Highly useful in studying the effect of factors like PCO2 , H+ concentration, etc., on binding of O2 with Hb.
- Factors favourable for dissociation of oxygen:
1. in the tissues,
2. low PO2
3. high PCO2
4. high H+ concentration
5. higher temperature
Bohr Effect:
Bohr discovered that Hb - O2 dissociation curve shift to right when CO2 tension is high in blood. It has concern with only blood CO2 (It has no relation with tissue fluid and alveoli CO2).
- PCO2 dissociation from oxy-Hb is directly proportion to blood PCO2.
- More PCO2 in blood means fast removal of O2 from OxyHB.
- When PC02 increases (blood pH decreases), Dissociation curve of OXY-Hb at 37*C shift to right side.
- Factors are favourable for the formation of oxyhaemcglobin.
- In Alveoli:
1. high PO2
2. low PCO2
3. lesser H+ concentration
4. lower temperature - This clearly indicates that O2 gets bound to hat and gets dissociated at the tissues.
- Every 100 ml of oxygenated blood can deliver around 5 ml of O2 to the tissues under normal physiological conditions.
Transport of CO2
- Due to CO2 solubility which is 20 times more than O2, its transport is much easier.
- 100ml of blood from tissue to lungs carry average 4 ml of CO2.
- Blood transport CO2 in three ways.
1. In dissolve state in plasma, blood plasma carries 7% of CO2 (0.3ml /100ml of blood).Oxygenated blood carry 2.4ml of CO2 in plasma while deoxygenated blood plasma carries 2.7ml in per 100 ml of blood.
2. In the form of bicarbonate ions, CO2 in plasma react with water and form carbonic acid. - This reaction is slow in plasma as it lacks Carbonic anhydrase but very fast in RBC as it has this enzyme,70% of the CO2 received by blood from tissue enter in RBC and form carbonic acid and immediately dissociate into hydrogen and bicarbonate ions.
- Here Hydrogen ions combine with Hb (reduced Hb) and maintain the blood pH 7.4 (otherwise blood become acidic) and bicarbonate ions diffuse in plasma from RBC and form sodium bi carbonate and to compensate it ,chlorides ions move into RBC to maintain electrostatic neutrality of plasma, some of the HCO3 remains in RBC and form KHCO3.
- Here movement of chloride ions from plasma into RBC is Chloride Shift/hamburger shift.
- HB is in reduced form.
- Hb is a powerful acid base buffer.
- In plasma, CO2 is present in form of sodium bicarbonate.
- In the form of carbamino compound:
- CO2 also directly react reversibly and loosely bound with Hb and form unstable compound called carbamino Hb and average 23% of CO2 receive from tissue fluid transported in this manner estimated 1ml CO2/100ml of blood.
- When PCO2 is high and PO2 is low as in the tissues → more binding of carbon dioxide occurs.
- So overall CO2 transportation in blood 1% in form of CO2, 23 % HHbCO2 and 7% HCO3 ions.
Haldane Effect/CO2 Diffusion at Alveoli
- It is promoting transportation of CO2. In the lungs, the Haldane effect release the CO2 and reason of this that formation of oxyHb which behave as strong acid and displaces CO2 from Carbamino Hb.
- It also releases Hydrogen ions from Hb (reduced Hb become oxidised here) and this ions combine with bicarbonate ions and form carbonic acid and dissociate into CO2 and H2O with help of carbonic anhydrase.
- In the lungs, release of CO2 from blood (due to oxyHb formation) while in the tissue it promotes CO2 uptake because of O2 dissociation from OXY-HB.
- At the tissue site, where PCO2 is high, CO2 diffuse into blood and form HCO3 -and H+ ions and at alveolar site PCO2 is lower, Formation of H2O and CO2 take place.
- Bohr effect promotes O2 transport while Haldane effect promotes CO2 transport.
Regulation of Respiration
- Ability to maintain and moderate the respiratory rhythm to suit the demands of the body tissues. → Done by the neural system.
- Respiratory rhythm centre → A specialised centre present in the medulla region of the brain which is primarily responsible for regulation of respiration. It has inspiratory area and expiratory area and inspiratory area is dominant over expiratory area.
- Respiratory movement is under control of medulla oblongata.
- Pneumotaxic centre Present in the pons region of the brain which moderate the functions of the respiratory rhythm centre. When this centre is stimulated, respiration rate increases inspiration and shortens the expiration through rhythm centre.
- Neural signal from this centre can reduce the duration of inspiration and thereby alter the respiratory rate.
- A Chemosensitive area situated adjacent to the rhythm centre.
- For detection of , 0 2 and hydrogen ion concentration following chemoreceptors are found.
- Peripheral Chemoreceptors - carotid body found in right and laft carotid artery and aortic body in arch of aorta detect decrease /increase of PO2 in atrial blood and send signal to respiratory centre for adjustment like low PO2 in blood, stimulate the inspiration.
- Central chemoreceptors - Located on ventral surface of medullaand take information from brain tissue fluid and Cerebro spinal fluid and send to respiratory center for action.Hydrogen ion concentration stimulate central chemoreceptor cells.
- Gasping center responsible for sudden and shallow respiration is located in pons.
- Apneustic center located in pons is for slow and deep respiration.
- Pneumotaxic centre located in pons is control other center and produce normal quite breathing.
- The role of oxygen in the regulation of respiratory rhythm is quite Insignificant.
- It is rise in rise in arterial CO2 and alveolar CO2 cause stimulation in respiratory center.
Disorders of Respiratory System
- Bronchial Ashthma: A difficulty in breathing causing wheezing. It is caused due to bronchial obstruction and spasm/contraction of smooth muscles due to inflammation of bronchi and bronchioles.
- Emphysema: A chronic disorder. Alveolar walls are damaged due to which respiratory surface is decreased. It is result into permanent short of breath. Major causes → cigarette smoking/air pollutant.
- Occupational Respiratory Disorders: In Cotton, Coal, grinding or stone-breaking industries → so much dust is produced → defence mechanism of the body cannot fully cope with the situation. Silicosis and Asbestosis are example of this. Long exposure → inflammation of lungs → leading to fibrosis (proliferation of fibrous tissues in upper part of lungs), lung damage.
- Common cold is caused due to rhinovirus in adult.
- Asphyxia: Suffocation is O2 content fall in blood.
- Hypoxia: Is condition of O2 shortage in blood.
Old NCERT Syllabus
- Pharynx: It is divided into three parts:
1) Nasopharynx - lt is upper part of pharynx in which internal nares open. It has 5 openings in its wall one pairs of internal nares,one pair of eustachian tube opening and one opening to oropharynx.
2) Oropharynx - ln this area oral cavity /Fauces open. It has two pair of tonsils that is palatine and lingual tonsils found.
3) Laryngiopharynx/Hypopharynx - lt leads into two tubes one at the front is wind pipe/Trachea for respiration and second is at the back is called oesophagus for food So oropharynx and laryngopharynx is for both food and air while nasopharynx is only for air. - Bronchioles: Bronchial epithelium has three type of cells:
1. Argentaffin /Kulchitsky cell secrets serotonin (constrict the bronchiole) and histamine (dilate the bronchiole).
2. Clara cells secretes surfactants which is phospholipid in nature which prevent the collapse of bronchioles which lack cartilaginous ring.
3. Dust cell which is phagocytic in nature and eat foreign particles. - Additional Infomation
- Cough is reflex action and its centre is medulla. It is occur when some food etc enter in. trachea and to expel them by coughing.
- Sneezing is also reflex action stimulated by epithelium of nasal chamber. It is forceful expiration.
- Hiccupping is noisy inspiration caused by muscular spasm of diaphragm at irregular interval.
- Yawning is prolonging inspiration in response of low 02 tension in blood. Mammals embryo respire through chorion.
- Aquatic salamander is lungless amphibians.
- SARS (severe acute respiratory syndrome) is caused by corona virus. It was originated from south china. Spreading of corona virus is from birds.
- It In pregnant women, breathing is done by intercostal muscles and diaphragm has no role.
FAQs on Key Notes: Breathing & Exchange of Gases - NEET
| 1. What is the process of breathing and exchange of gases in the human body? |  |
Ans. Breathing, also known as respiration, is the process of inhaling oxygen and exhaling carbon dioxide. It involves the exchange of gases between the lungs and the environment. When we inhale, the diaphragm and intercostal muscles contract, causing the chest cavity to expand. This results in the intake of air into the lungs. Oxygen from the inhaled air is then transferred to the bloodstream through tiny air sacs called alveoli. At the same time, carbon dioxide, a waste product, is released from the bloodstream into the lungs and exhaled during exhalation.
| 2. How does oxygen reach the body's cells after being inhaled? |  |
Ans. After being inhaled, oxygen enters the bloodstream through the alveoli in the lungs. It binds to hemoglobin, a protein found in red blood cells, forming oxyhemoglobin. This oxygen-rich blood is then pumped by the heart to various parts of the body through arteries. As the blood reaches the body's tissues and organs, the oxygen is released from the oxyhemoglobin and diffuses into the cells. This oxygen is then utilized by the cells for various metabolic processes, including energy production.
| 3. What happens to carbon dioxide in the body during the process of respiration? |  |
Ans. During respiration, carbon dioxide is produced as a waste product of cellular metabolism. It diffuses from the cells into the bloodstream and is transported back to the lungs. In the lungs, carbon dioxide is excreted from the body through exhalation. The process of exhalation involves the relaxation of the diaphragm and intercostal muscles, causing the chest cavity to contract and push air out of the lungs. This allows for the removal of carbon dioxide from the body and the replenishment of oxygen through inhalation.
| 4. How does the body regulate the exchange of gases during respiration? |  |
Ans. The exchange of gases during respiration is regulated by various mechanisms in the body. The concentration of oxygen and carbon dioxide in the bloodstream is monitored by chemoreceptors located in the brain and blood vessels. If the oxygen levels decrease or carbon dioxide levels increase, these chemoreceptors send signals to the respiratory center in the brain, which then increases the rate and depth of breathing. This helps to increase the intake of oxygen and removal of carbon dioxide, ensuring a proper exchange of gases in the body.
| 5. What are some common respiratory disorders that can affect the breathing and exchange of gases? |  |
Ans. There are several respiratory disorders that can affect the breathing and exchange of gases in the body. Some common examples include asthma, chronic obstructive pulmonary disease (COPD), pneumonia, and bronchitis. These conditions can cause narrowing of the airways, inflammation, mucus buildup, and difficulty in the exchange of gases. They can lead to symptoms such as shortness of breath, wheezing, coughing, and reduced oxygen levels in the bloodstream. Treatment for these disorders may involve medications, inhalers, oxygen therapy, and lifestyle modifications.
Related Searches















