Food & Nutritions Problems | Geography Optional for UPSC PDF Download
Introduction
In the previous unit, we learned about the importance of macronutrients and micronutrients in our diet. Macronutrients include carbohydrates, fats, and proteins, while micronutrients consist of vitamins and minerals. In this unit and the next, we will explore the diseases that can occur when there is a deficiency of these essential nutrients in the body.
Nutritional deficiencies are a significant concern in India, especially in rural areas and among poor families. You may have encountered reports or articles about nutritional disorders caused by a lack of macronutrients, such as energy and protein, or micronutrients like vitamin A and B complex.
Human beings need a balanced diet to live, thrive, and perform various activities. Any imbalance or inadequacy in food and nutrients can lead to poor health, nutritional disorders, and even death. This unit focuses on nutritional problems that have public health implications.
Protein Energy Malnutrition (PEM)
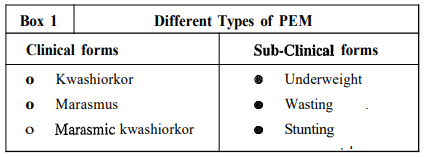
Protein Energy Malnutrition (PEM) refers to the deficiency of macronutrients, specifically energy and protein, in the diet. It is a significant public health concern and affects all segments of the population, including children, women, and adult men, particularly in backward and marginalized communities.There are various forms of PEM, ranging from severe, clinically detectable cases to milder forms where growth retardation is the primary symptom. PEM is prevalent in developing countries, particularly in Asia and Africa, with a substantial number of children affected globally.
Different Forms of PEM
PEM is clinically distinguishable into three main forms:- Kwashiorkor
- Marasmus
- Marasmic-Kwashiorkor
In addition to these clinical forms, many children suffer from sub-clinical forms of PEM, such as underweight, stunting (short stature), and wasting (thinness). The prevalence of clinical cases in a community often represents only a small fraction of the actual number of children affected by sub-clinical PEM.
Types of Protein-Energy Malnutrition (PEM)
- Kwashiorkor: This is a severe form of protein deficiency, often occurring in children who have a diet low in protein but not necessarily low in calories. It is characterized by symptoms such as swelling (edema), irritability, and skin changes.
- Marasmus: This form results from a severe deficiency of both protein and calories. It is marked by extreme thinness, loss of muscle mass, and a general wasting away of body tissues.
- Marasmic-Kwashiorkor: This is a combination of both Kwashiorkor and Marasmus, where a child exhibits symptoms of both forms.
Kwashiorkor
The term "kwashiorkor" comes from an African word that means "disease of the displaced child," highlighting the condition's link to inadequate nutrition.
- Kwashiorkor is a severe form of protein-energy malnutrition (PEM) where the body does not get enough protein.
- It mainly affects children between the ages of 1 and 3 years, especially when they are weaned off breast milk.
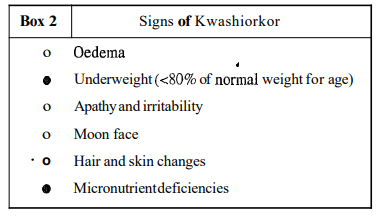
- The key signs of kwashiorkor include:
- Oedema (swelling of the feet)
- Growth failure (stunted growth)
- Mental changes (altered behaviour and mood)
- Oedema. This is the buildup of fluid in the body's tissues, starting with swelling in the feet and spreading to the legs, hands, and face. Pressing on swollen areas leaves a dent, indicating oedema.
- Poor growth. Children with kwashiorkor are significantly lighter and shorter than their peers, weighing 80% or less of the normal weight for their age.
- Mental changes. Affected children may appear apathetic, irritable, and prefer to stay in one place.
- Hair changes. Hair becomes thinner, silkier, and takes on a coppery red colour. Hair can be easily pulled out without pain.
- Skin changes. Dermatosis, or skin changes, occur, particularly in areas of friction. Patches of dark, pigmented skin may develop, resembling sunburn.
- Moon face. The face may appear swollen, particularly the cheeks, due to fluid or fatty tissue.
- Micronutrient deficiencies. Most children have some degree of anaemia (iron deficiency), and signs of vitamin A and B complex deficiencies are common.
- Water and electrolyte imbalance. Total body water is increased, especially extracellular fluid. There may be signs of dehydration, such as sunken eyes and dry mucosa. Sodium levels may be increased, while potassium and magnesium levels are often deficient.
- Infections. Lower respiratory tract infections, often associated with diarrhoea or dysentery, may be present.
Marasmus
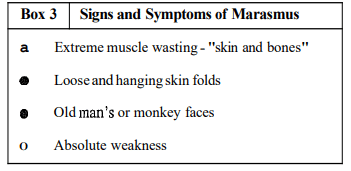
Marasmus is a severe form of malnutrition that typically occurs in children under the age of 2. It is characterized by extreme emaciation, with the child appearing as nothing but "skin and bones." Unlike kwashiorkor, marasmus does not involve edema or changes in skin and hair.
- Severe growth retardation
- Underweight. < 40% of normal weight for age)
- Apathy and irritability
- Moon face
- Hair and skin changes
- Micronutrient deficiencies
- Old man's or monkey's face
- Loose and hanging skin folds over arms and buttocks
Marasmus is a condition that occurs at the other end of the spectrum from kwashiorkor. It is commonly seen in children under the age of 2 years. The characteristic signs and symptoms of marasmus include:
- Severe growth retardation: Children with marasmus experience significant delays in growth and development.
- Underweight: These children weigh less than 40% of the normal weight for their age, indicating extreme malnutrition.
- Apathy and irritability: Affected children may appear lethargic and irritable due to their weakened state.
- Moon face: Some children with marasmus may develop a rounded face, similar to the appearance seen in kwashiorkor.
- Hair and skin changes: There may be alterations in the texture and appearance of hair and skin, although these changes are not as pronounced as in kwashiorkor.
- Micronutrient deficiencies: Children with marasmus often suffer from deficiencies in essential micronutrients, such as vitamin A, iron, and B-complex vitamins.
In addition to these signs, marasmic children are extremely weak and lack subcutaneous fat, with loose skin folds, particularly over the buttocks. When held in a standing position, the loose skin folds are prominently visible. For their age, these children typically fall below 60% of the normal weight or < Median - 3SD of the standards. Frequent episodes of diarrhea leading to dehydration are common in marasmus.
Marasmic Kwashiorkor
Signs and Symptoms of Marasmus
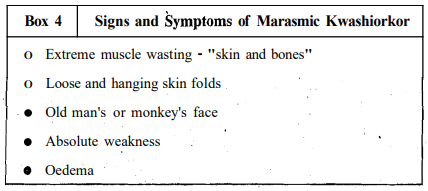
In regions where Protein-Energy Malnutrition (PEM) is prevalent, some malnourished children may display characteristics of both kwashiorkor and marasmus. This can occur during the transition from one form of severe PEM to another. For instance:
- A child with marasmus might develop oedema following a severe infection.
- Conversely, a child with kwashiorkor, upon losing oedema, may develop marasmic features.
When a child exhibits signs of extreme wasting (indicative of marasmus) along with oedema (a sign of kwashiorkor), they are described as suffering from "marasmic kwashiorkor." These children may also show hair changes and often experience diarrhoea.
This phenomenon illustrates a continuous spectrum of signs, ranging from oedematous kwashiorkor to varying degrees of marasmus associated with oedema. For reference, we have included the main features of PEM in children.
- In addition to the key features highlighted in Table 3.1, various biochemical changes occur in blood, urine, gastrointestinal secretions, endocrine functions, and tissue composition related to Protein-Energy Malnutrition (PEM).
- The most significant changes that are crucial for diagnosis and treatment of PEM are summarized below.
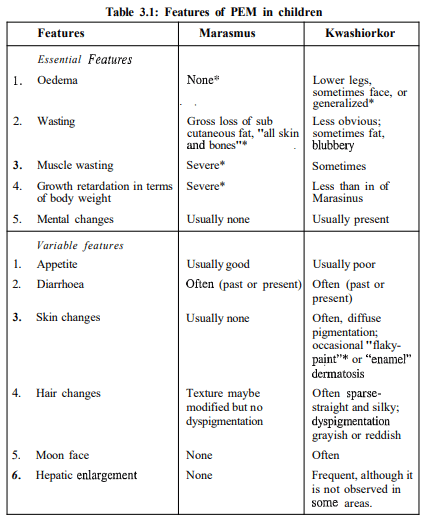
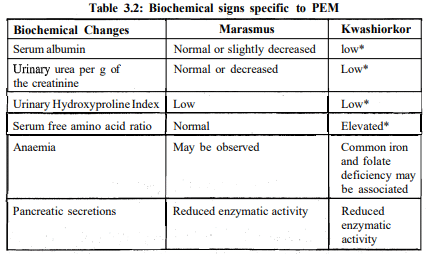
- In Table 3.2, it is clear that both serum albumin and serum total protein levels are significantly low in cases of kwashiorkor.
- The level of serum albumin is one of the best measures of protein-energy malnutrition (PEM).
- We will explore this important indicator more in Unit 9.
- Regarding urine changes, the amount of hydroxyproline found in urine is suggested as a sign of how quickly children with PEM are growing.
- This index remains fairly stable from 6 months to about 5 years of age.
- Children who are malnourished show low levels of hydroxyproline in their urine.
- Additionally, the urinary excretion of creatinine decreases as muscle mass reduces.
- Therefore, both in kwashiorkor and marasmus, creatinine levels in urine are low.
- We have discussed the clinical types of PEM. Now, we will look into sub-clinical PEM.
Protein-Energy Malnutrition (PEM)
In rural India, clinical forms of Protein-Energy Malnutrition (PEM) represent only a small fraction of the total cases. Growth retardation is a key indicator of PEM and also the first sign of recovery when rehabilitation begins. Anthropometry, or body measurement, is widely used to detect various degrees of sub-clinical PEM, with body weight being the most sensitive and commonly used indicator of nutritional status, especially in preschool children aged 1 to 5 years.
Several methods exist for classifying PEM in children, either based on body weight alone or in combination with height or length. The following classifications based on body weight are commonly used in India:
- Gomez classification
- Indian Academy of Pediatrics (IAP) classification
- Standard deviation classification
Gomez Classification:
The Gomez classification was proposed by a child specialist named Gomez in Mexico. He and his team suggested categorizing the body weights of children as a percentage of normal values (standards) for their age. They identified four grades of malnutrition based on this approach. Gomez observed significant differences in mortality rates between children with second and third-grade malnutrition, highlighting the importance of this classification in prioritizing actions for intervention.
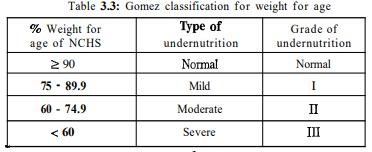
Gomez Classification for Weight for Age:
- The Indian Academy of Pediatrics (IAP) has proposed a classification system for grouping children into various grades of malnutrition based on weight for age.
- This classification is widely used in India and forms the basis for growth charts used in national nutrition intervention programs like the Integrated Child Development Services (ICDS).
- According to the IAP classification, children with body weights more than 80% of the National Center for Health Statistics (NCHS) standards are considered normal.
- The classification includes different grades of undernutrition, ranging from normal to severe.
Standard Deviation and Classification of Undernutrition:
- Statistics indicates that when normal values of any variable are distributed according to their frequency of occurrence, they follow a normal distribution within two standard deviations (SD) of the mean or median.
- Based on this principle, children with weights less than median -2SD of normal weight for age (NCHS standards) are considered to be suffering from undernutrition.
- The criteria for classifying children into various degrees of undernutrition are based on mean, median, and standard deviation.
Prevalence of Protein-Energy Malnutrition
Prevalence Rate indicates the number of individuals with a particular disease at a specific time in a defined population (usually per 100 people).
Decline in Prevalence. In the early 1960s, the prevalence of kwashiorkor and marasmus was around 4%. This has significantly declined over the years. Recent surveys by the National Nutrition Monitoring Bureau (NNMB) show that the prevalence of these conditions is now about 1%.
- Sub-clinical PEM. Despite the low prevalence of kwashiorkor and marasmus, approximately half of children under 5 years old suffer from sub-clinical Protein-Energy Malnutrition (PEM) when assessed by weight for age.
- Stunting. About 60% of these children are also stunted, indicating short stature for their age.
Underweight Statistics. The National Family Health Survey reveals that around 47% of children under 3 years old, who are at risk of developing PEM, are underweight.
Widespread Issue. These statistics indicate that PEM is a widespread problem in India, affecting a significant portion of the population, and necessitating immediate intervention and action.
Causes of Protein-Energy Malnutrition (PEM)
Protein-Energy Malnutrition (PEM) in children has several contributing factors, especially in rural India. Let's explore these causes in detail:Low Birth Weight:
- Many children in rural India are born with low birth weights (less than 2.5 kg) due to high maternal malnutrition. A normal birth weight ranges from 3 to 3.4 kg. This low birth weight is a significant factor in the early onset of PEM.
Inadequate Breast Milk:
- While prolonged breastfeeding is common in rural India, the quantity of breast milk produced by malnourished mothers is often insufficient. This leads to inadequate nutrition for infants, as they do not receive enough breast milk to meet their needs.
Delayed Complementary Feeding:
- In poorer socioeconomic groups, there is a common practice of delaying the introduction of complementary foods (foods in addition to breast milk) until the child is about one year old. This delay exacerbates dietary inadequacy, especially when breast milk is already insufficient. After weaning, children are often given adult diets, which young infants cannot consume in adequate amounts due to their bulk.
Early and Abrupt Weaning:
- Early and sudden weaning, along with the introduction of diluted milk formulas, can lead to conditions like marasmus, a severe form of malnutrition.
Primarily Energy Deficiency:
- Surveys indicate that PEM is primarily due to dietary energy deficiency resulting from insufficient food intake. The main issue in the diets of Indian children, which are often based on cereals and pulses, is energy deficiency rather than protein deficiency, which was previously believed.
Infections and Infestations:
- Childhood infections (both viral and bacterial) and parasitic infestations are commonly associated with PEM. These conditions can lead to anorexia (loss of appetite), reduce nutrient absorption and utilization, and result in nutrient losses. Infections like measles, frequent diarrhoea, and acute respiratory infections play a crucial role in the onset of PEM.
Ignorance and Poor Socioeconomic Status:
- Improper childcare due to lack of knowledge or time contributes to the onset of PEM. It is primarily a condition affecting the poor and marginalized. Mothers in these families may be illiterate, work long hours, and be influenced by societal beliefs, superstitions, and spiritual healing practices. Even if these families spend their entire income on food, their low purchasing power prevents them from meeting nutritional requirements.
These factors collectively contribute to the prevalence of Protein-Energy Malnutrition in children, highlighting the need for improved maternal nutrition, healthcare, and education in rural areas.
Consequences of PEM
- Irreversible Growth Retardation: PEM can lead to permanent stunted growth.
- Increased Susceptibility to Infections: Children with PEM have a weakened immune system, making them more prone to infections.
- Increased Risk of Mortality: The risk of death is higher in children with moderate to severe PEM, especially when they are exposed to frequent infections.
- Low Cognitive Performance: PEM can negatively impact cognitive abilities, affecting learning and development.
- Low Purchasing Power: Families with low income may struggle to provide adequate nutrition, contributing to PEM.
- Food Taboos and Superstitions: Cultural beliefs about food can lead to dietary inadequacies, increasing the risk of PEM.
- Large Families: In large families, resources may be stretched thin, leading to insufficient nutrition for all members.
- High Female Illiteracy: Lack of education among women can impact their ability to provide proper nutrition for their children.
In India, extensive PEM since early childhood has resulted in irreversible growth retardation, leading to short stature among adults. While children from well-off communities are as tall and heavy as those from developed countries, poorer children suffer from stunting, wasting, and underweight. Studies show that children with various grades of PEM have reduced immunity, making them more susceptible to infections like diarrhea and respiratory infections.
Treatment of PEM
The main goal in treating PEM is to ensure sufficient energy and protein intake while managing any infections. Mild and moderate cases can be treated at home under health professional supervision, but severe cases, especially with serious infections, require hospital referral.Key Aspects of Treatment for Severe PEM:
1. Dietary Intervention:
- Provide a diet rich in energy and protein, exceeding normal requirements for rapid recovery.
- Recommended Intake: Energy: 170-200 kcal per kg of body weight Protein: 3-4 g/kg of body weight
- Initial Diet: Start with a milk-based liquid diet using fresh milk or dry skimmed milk powder.
- Example Milk Formula: 90 g dried skimmed milk powder, 70 g sugar, 50 g vegetable oil in 1 litre of water.
- Feeding Guidelines: 100-150 ml of reconstituted formula per kg of body weight.
- Vitamin A Supplement: Since dried skimmed milk powder lacks vitamin A, supplement it.
- Gradual Introduction of Solid Foods: As appetite improves, gradually introduce solid foods.
- Special Diets for Older Children: Cereal, pulse, dried skimmed milk powder, and sugar/jaggery with added vegetable oil for energy density.
2. Vitamin and Mineral Supplements:
- Provide multivitamin preparations to meet increased recovery demands.
- Iron (60 mg) and Folic Acid (100 mg): Administer daily to correct anemia.
3. Oral Rehydration:
- Correct dehydration due to diarrhea with homemade or commercial oral rehydration solutions.
- WHO ORS Formula: Sodium chloride: 3.5 g, sodium bicarbonate: 2.5 g, potassium chloride: 1.5 g, glucose: 20 g dissolved in 1 litre of water.
- Administer ORS at 70-100 ml/kg body weight; intravenous fluids for severe dehydration.
4. Infection and Infestation Control:
- Start appropriate antibiotics immediately to combat infections, a leading cause of death in these children.
- Treat intestinal infestations such as giardiasis and ascariasis.
5. Monitoring Clinical Progress:
- Expect clinical improvement within a week with reduced edema and improved appetite.
- Weight gain typically follows after initial weight loss.
- Involve mothers in diet preparation to ensure proper nutrition post-hospitalization.
Prevention and Control of Protein-Energy Malnutrition (PEM)
To prevent and control PEM, a holistic and comprehensive approach is necessary, considering the family as a unit and adopting a life cycle approach.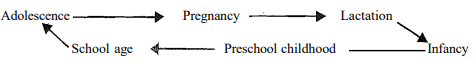
Here are some key measures:
- Ensure Proper Diet: Adequate quantities of a well-balanced diet containing all essential nutrients should be provided daily. Communities need to be made aware of the importance of feeding their children and family members adequately.
- Increase Purchasing Power: Socio-economic development aimed at poverty alleviation and increasing the purchasing power of the rural and urban poor is crucial.
- Supplementary Feeding: Programs like the Integrated Child Development Services (ICDS) provide daily supplementary food to children in poor rural families, offering about 300 kcal of energy and 8-10 g of protein per child.
- Promoting Food Security: Public distribution of food grains through ration shops, especially to the population below the poverty line, to improve food and nutrition security.
- Poverty Alleviation: Development programs aimed at providing employment assurance to the landless and other laborers to increase their purchasing power.
- Behavioral Change Communication: Educating and changing the behavior of women, particularly mothers, regarding proper diet and intrafamily food distribution through communication programs, cooking demonstrations, and mass media.
It is essential to address both direct nutrition interventions and underlying socio-economic factors to effectively prevent and control PEM.
Micronutrient Deficiencies
In the previous section, we learned about macronutrient deficiencies, particularly protein-energy malnutrition in children. We now understand that this is a significant public health issue affecting millions of young Indian children from impoverished rural communities. In addition to this, deficiencies in specific micronutrients such as vitamin A, iron, and iodine impact large segments of the population. Micronutrients are essential for maintaining normal metabolism and function, even though they are required in minute quantities. Some people refer to them as "super nutrients" to highlight their importance and the serious consequences of their deficiencies.Among all micronutrient deficiencies, those of vitamin A, iron, and iodine are particularly detrimental, affecting millions and contributing to high morbidity and mortality rates. Deficiencies in other micronutrients such as zinc, selenium, and molybdenum, while not manifesting as obvious problems, can lead to functional changes in the body.
Vitamin A Deficiency
- Vitamin A deficiency (VAD) is a significant public health issue, particularly affecting preschool children and pregnant women in low-income countries. In children, VAD is the leading cause of preventable severe visual impairment and blindness.
- An estimated 250,000 to 500,000 children with VAD worldwide go blind each year, and about half of them die within a year. Vitamin A is crucial for maintaining healthy epithelial tissue and normal vision. A deficiency in vitamin A manifests as eye lesions grouped under the term "xerophthalmia." These lesions can range from mild conditions, such as night blindness and changes in the conjunctiva (the white part of the eye), to severe cases that damage the cornea (the transparent front part of the eye), leading to irreversible blindness.
In this section, we will explore the ocular manifestations, prevalence, causes, treatment, and prevention of vitamin A deficiency.
Night Blindness:
- Night blindness is the earliest symptom of vitamin A deficiency. When the supply of vitamin A aldehyde (retinal) to the rod cells of the retina is reduced, dark adaptation is impaired.
- This means that the affected child has difficulty seeing in low light conditions, especially after sunset. For example, a mother might notice her child's inability to see food or toys in a dimly lit room. Pregnant women can also experience symptoms of deficiency, such as night blindness, which may continue into the early period of lactation. In some regions, there is a local term for this condition; in Hindi, it is called "Rathaundi."
Bitot's Spots:
- As vitamin A deficiency progresses, dirty white, foamy, and raised spots develop on the surface of the conjunctiva, usually on the outer side of the cornea.
- These spots are caused by the accumulation of denuded conjunctival epithelial cells. When treated with "Kajal," these spots stain black in the eyes. They are superficial and can be easily removed by direct inking or by crying in a child.
Conjunctival Xerosis:
- Conjunctival xerosis is characterized by dryness of the conjunctiva, which becomes thick, rough, and wrinkled. In a normal child, the conjunctiva is bright white, smooth, and glistening.
- However, in a child with conjunctival xerosis, the conjunctiva shows changes such as dryness, unwettability, loss of transparency, wrinkling, and pigmentation.
Corneal Xerosis:
- Corneal xerosis is a sign of severe vitamin A deficiency, where the cornea loses its normal smooth and glistening appearance, becoming dry and rough.
- Children with this condition may keep their eyes closed, especially in bright light due to photophobia (sensitivity to bright light), which can lead to missed diagnoses during clinical examinations.
Corneal Ulcer:
- If corneal xerosis is not treated promptly, it can lead to corneal ulceration. Initially, the ulcer may be shallow, but if it deepens, it can result in perforation and prolapse of the eyeball's contents.
- These lesions are more commonly found in the lower central cornea.
Keratomalacia:
- Keratomalacia is a condition characterized by the rapid destruction and liquefaction of the full thickness of the cornea, leading to iris prolapse and permanent blindness.
- It typically involves softening of the entire thickness or, more often, the whole cornea, resulting in deformation or destruction of the eyeball. The process is painless, but the corneal structure melts into a cloudy gelatinous mass, which can be dead-white or dirty yellow in color. In some cases, the lens and vitreous may be extruded. In infectious conditions, the eye may appear red and swollen.
Corneal Scar:
- Corneal ulcers, when healed, leave behind white scars that vary in size depending on the size of the ulcer. If the scar is large or positioned centrally, blocking the pupillary region, it can affect normal vision.
The thickening of hair follicles, known as follicular hyperkeratosis, is a skin condition that can occur due to a lack of vitamin A.
- Xerophthalmia is an eye condition that results from not having enough vitamin A.
- This condition includes various symptoms that we have discussed earlier.
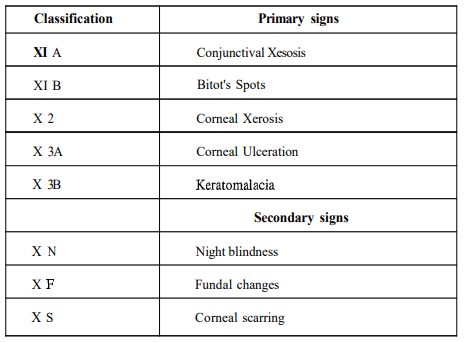
- The World Health Organization (WHO) classifies these symptoms, which are summarized in a table.
Iron Deficiency Anaemia (IDA)
- Iron deficiency anaemia (IDA) is the most widespread micronutrient deficiency globally, especially in developing nations like India.
- It is estimated that about 4-5 billion people, or 66-80% of the world's population, may be lacking in iron.
- Approximately 2 billion people, which is over 30% of the global population, are affected by anaemia.
- Anaemia happens when haemoglobin, the pigment that gives red blood cells their color, is produced at a significantly lower level, resulting in reduced haemoglobin in the blood.
- Most cases of anaemia are caused by iron deficiency; however, other reasons can include folate and vitamin B12 deficiencies or chronic diseases.
- Iron deficiency and anaemia can lower the work capacity of individuals and entire populations, leading to serious economic issues and hindering national development.
- For children, the health impacts can include:
- Premature birth
- Low birth weight
- Increased risk of infections
- Higher chances of death
- Impaired physical and cognitive development, which can lead to poor school performance
- For pregnant women, anaemia is linked to 20% of all maternal deaths.
- Iron deficiency affects more individuals than any other health condition, making it a significant public health issue.
- Now, let’s look at the signs and symptoms of IDA:
- Due to reduced haemoglobin levels, affected individuals may experience pallor (paleness) in various body parts, especially noticeable in the conjunctiva of the eyes and the roof of the mouth.
- Anaemic individuals often experience breathlessness even with minimal physical activity, as haemoglobin is essential for transporting oxygen in the body.
- These symptoms are particularly prominent in adults, especially pregnant and lactating women.
- The nails on fingers and toes may become thin and curve upwards, a condition known as koilonychia.
- In severe cases, especially among pregnant women, swelling in the feet, known as oedema, can occur.
- The best way to diagnose anaemia is through a blood test that measures haemoglobin levels.
Treatment of Iron Deficiency Anaemia
Consequences of Iron Deficiency Anaemia
Oral Iron Supplementation:
- Oral iron is the preferred treatment for Iron Deficiency Anaemia (IDA).
- Dosage depends on the severity of the condition.
- Generally, for moderate to severe anaemia, 2 tablets of fersolate (each containing 100 mg of elemental iron) are recommended.
Side Effects and Management:
- Common side effects include gastric irritation, constipation, black stools, and sometimes joint pains, which can lead to patients discontinuing treatment.
- To mitigate these side effects, patients should be advised to take the tablets after food.
Severe Cases:
- In very severe anaemia with extremely low haemoglobin levels (< 5-7 g/100 ml), packed cell transfusion is recommended.
- This treatment should be considered only after a thorough evaluation of the patient.
- Parenteral iron therapy may be advised when oral iron is not tolerated or in late pregnancies.
- Due to the risk of systemic and allergic reactions, parenteral iron should preferably be administered in hospitals.
Consequences of Iron Deficiency Anaemia:
- Maternal and Perinatal Mortality: Iron deficiency anaemia can lead to increased risks of maternal and perinatal mortality.
- Low Birth Weight and Prematurity: Infants born to mothers with iron deficiency anaemia are at higher risk of low birth weight and prematurity.
- Reduced Physical Work Capacity: Individuals with iron deficiency anaemia may experience reduced physical work capacity.
- Poor Cognitive Performance in Children: Children who were born to mothers with iron deficiency anaemia may exhibit poor cognitive performance.
Importance of Prevention:
- Given the prevalence of iron deficiency anaemia, especially among women and children, it is crucial to focus on preventive measures.
Prevention of Iron Deficiency Anaemia
- Dietary Improvement: Long-term correction of dietary inadequacy is crucial for preventing iron deficiency anaemia. This involves increasing the availability of iron-rich foods in the diet and changing community behaviours towards food consumption.
- Supplementation: Iron supplementation is necessary for specific groups to prevent anaemia. This includes the consumption of iron and folic acid tablets, especially for pregnant women, lactating women, preschool children, and family planning acceptors.
- Food Fortification: Fortifying commonly consumed food items with iron can help prevent deficiency. Suitable vehicles for fortification include iodized salt, wheat flour, and breakfast cereals.
- Dietary Diversification: Ensuring access to iron-rich foods and foods high in vitamin C (which aids iron absorption) is important. Promoting home gardening and horticulture can help communities access these foods.
- Education and Behaviour Change: Raising awareness and changing behaviours regarding dietary practices and the importance of iron-rich foods are essential for long-term prevention.
- Health Care: Improving health care access and education to ensure proper implementation of nutritional programmes and dietary recommendations.
Despite the launch of the 'National Nutritional Anaemia Control Programme' in 1970, the prevalence of anaemia remains high due to poor implementation and other challenges.
Iodine Deficiency Disorders
Iodine is a crucial micronutrient necessary for the proper mental and physical growth and development of humans. However, iodine deficiency is a widespread issue present in many parts of the world. Iodine Deficiency Disorders (IDD) impact over 740 million people, which is about 13% of the global population, with an additional 30% at risk. In India, approximately 60 million people are expected to suffer from goitre, and another 3 million from cretinism due to iodine deficiency. Around 200 million people in the country are at risk of developing IDD.
Endemic Goitre Belt
- Traditionally, the endemic goitre belt in India spans the entire sub-Himalayan region, from Jammu and Kashmir to Arunachal Pradesh.
- Recently, new regions have been identified as affected by iodine deficiency, including parts of Andhra Pradesh, Karnataka, Kerala, Maharashtra, and Madhya Pradesh.
Spectrum of Iodine Deficiency Disorders
- IDD encompasses a range of disabling conditions that impact human health from fetal development through adulthood, resulting from inadequate dietary intake of iodine.
- The thyroid gland produces thyroxine, a hormone vital for various bodily functions. When iodine intake falls below recommended levels, the thyroid gland struggles to produce sufficient amounts of this hormone.
Goitre:
- One of the most noticeable features of iodine deficiency disorders is goitre.
- When there is a deficiency of iodine, the thyroid gland enlarges in an attempt to produce the necessary thyroxine hormone, leading to swelling.
- This condition is known as goitre and is not merely a cosmetic issue; it reflects a serious underlying health problem related to thyroid function.
Effects of Iodine Deficiency in Mothers and Infants:
- Iodine deficiency in pregnant women can severely impact the development of the unborn child.
- It may lead to miscarriages, congenital defects, and higher perinatal mortality rates.
- One of the most severe consequences of fetal iodine deficiency is endemic cretinism, characterized by stunted growth, intellectual disabilities, deaf-muteness, and spastic paralysis of the legs.
Hypothyroidism and Iodine Deficiency:
- Insufficient production of thyroid hormone due to iodine deficiency leads to hypothyroidism.
- Hypothyroidism is a major factor contributing to damage in the developing brain and other adverse effects collectively referred to as iodine deficiency disorders (IDD).
Cognitive and Behavioral Effects:
- Populations living in iodine-deficient areas often exhibit lower intelligence, lack of initiative, and poor decision-making abilities.
Prevalence of Iodine Deficiency Disorders (IDD)
Manifestations of IDD
- The prevalence of Iodine Deficiency Disorders (IDD) can be determined through population surveys, which primarily focus on the clinical assessment of goitre and cretinism, the two classical features of iodine deficiency.
- Goitre, an enlargement of the thyroid gland, is a key indicator of IDD. To assess the size of goitre clinically, a standard technique involving the palpation of the thyroid gland is used.
- The World Health Organization (WHO) has established criteria for the classification of goitre size, which is crucial for determining the Total Goitre Rate (TGR).
- The TGR is calculated by summing the grades of goitre size, specifically grades 1 and 2. IDD is considered a public health problem when the TGR exceeds 10% among children aged 6-12 years in a given area.
Consequences of IDD
- Mental Retardation
- Defects in Nervous System Development
- Goitre
- Physical Sluggishness
- Growth Retardation
- Reproductive Failure
- Increased Childhood Mortality
- Lowered Economic Productivity
Cretinism is a severe condition resulting from iodine deficiency during pregnancy, which negatively impacts fetal thyroid function. There are two main types of cretinism:
- Neurological Cretinism: This type is more common and is characterized by poor cognitive abilities, deaf mutism, speech defects, and proximal neuromotor rigidity.
- Myxoedematous Cretinism: This type includes hypothyroidism with dwarfism and is less prevalent.
Maternal iodine deficiency during pregnancy is linked to a higher risk of stillbirths, abortions, and congenital abnormalities. Iodine deficiency is considered the leading cause of preventable mental retardation worldwide.
Prevention of IDD
- Iodized Salt Distribution: Fortifying common salt with potassium iodate is the most common and oldest control measure. In India, the effectiveness of iodized salt in controlling endemic goitre was first proven in the Kangra Valley of Himachal Pradesh. This led to the launch of the National Goitre Control Programme in 1962 by the Government of India to supply iodized salt in endemic areas.
- Communication Campaign:. mass communication campaign is necessary to raise awareness in the community about the consequences of IDD and the benefits of iodized salt. People should be informed about the harmful effects of iodine deficiency and encouraged to consume iodized salt daily.
- Double Fortified Salt: Simultaneous fortification of salt with iron and iodine is an effective approach to control both iron deficiency anemia and iodine deficiency disorders. The technology for double fortification of salt has been developed at NIN, and community trials are underway for field-testing.
- Iodized Oil: In hyper-endemic areas, intramuscular injection of iodized oil has been used to tackle goitre and cretinism. A single dose of 1 ml can provide protection for 3-5 years. However, the high cost and difficulty in reaching all victims make this approach less practical. The use of disposable syringes is now mandatory due to the risk of hepatitis-B and HIV/AIDS.
Zinc Deficiency
- Zinc is an essential trace element that plays a crucial role in various biological functions. It is a cofactor for over 200 metalloenzymes that regulate cellular processes such as cell division, growth, immune function, and protection against free radical damage.
- Zinc deficiency can lead to a range of health issues, especially in vulnerable populations such as preschool children in lower-income countries.
Consequences of Zinc Deficiency
Signs and Symptoms:
- Poor Appetite: One of the earliest signs of zinc deficiency, leading to growth issues.
- Skin Lesions: Characteristic manifestations of zinc deficiency.
- Hair Loss (Alopecia):. common symptom associated with zinc deficiency.
- Failure to Thrive: Growth retardation and developmental delays.
- Diarrhea: Particularly prominent in infants up to 2 months of age with zinc deficiency.
- Cognitive Impairments: Early zinc deficiency can lead to problems with cognitive function, behavioral issues, mood changes, memory impairment, and spatial learning difficulties.
- Recurrent Infections: Increased susceptibility to infections due to compromised immune function.
- Blepharoconjunctivitis: Inflammation of the eyelids and conjunctiva, commonly seen in school-aged children with zinc deficiency.
Pathological Conditions:
- Zinc deficiency can occur in various pathological conditions such as:
- Chronic Alcoholic Liver Disease: Impaired zinc metabolism and absorption.
- Sickle Cell Disease: Increased zinc requirements and/or decreased absorption.
- Chronic Malabsorption Syndromes: Conditions like celiac disease that affect zinc absorption.
Age-Related Variations:
- The severity and manifestations of zinc deficiency can vary with age:
- Infants: Diarrhea is a prominent symptom in infants up to 2 months of age.
- School-Aged Children: Common findings include alopecia, growth retardation, blepharoconjunctivitis, and recurrent infections.
- Elderly: Chronic non-healing leg ulcers and recurrent infections may occur.
Maternal Zinc Deficiency:
- Adverse consequences of maternal zinc deficiency during pregnancy include:
- Intrauterine Growth Retardation: Poor fetal growth in utero.
- Low Birth Weight: Infants born with low birth weight.
- Poor Fetal Neurobehavioral Development: Impaired development of the fetal nervous system.
- Increased Neonatal Morbidity: Higher rates of illness in newborns.
Maternal Outcomes:
- Adverse maternal outcomes associated with zinc deficiency include:
- Preterm Delivery: Giving birth before 37 weeks of gestation.
- Pregnancy-Induced Hypertension: High blood pressure during pregnancy.
Recommended Daily Requirements:
- The recommended daily allowances (RDAs) for zinc vary by age, sex, and life stage.
- Infants: 2-5 mg/day, depending on age.
- Children: 5-10 mg/day, depending on age.
- Adults: 10-15 mg/day, with higher requirements for pregnant and lactating women.
|
303 videos|636 docs|252 tests
|
FAQs on Food & Nutritions Problems - Geography Optional for UPSC
| 1. What is Protein Energy Malnutrition (PEM) and how does it affect individuals? |  |
| 2. What are the main causes of Protein Energy Malnutrition (PEM)? |  |
| 3. What are the consequences of Protein Energy Malnutrition (PEM) on health? |  |
| 4. How is Protein Energy Malnutrition (PEM) treated? |  |
| 5. What measures can be taken to prevent and control Protein Energy Malnutrition (PEM)? |  |





















