Vitiligo | Medical Science Optional Notes for UPSC PDF Download
| Table of contents |

|
| Hypo pigmented patches-Differential diagnosis |

|
| Vitiligo-Etiology |

|
| Vitiligo-Etiology (Theories) |

|
| Clinical Classification |

|
| Vitiligo-Diagnosis |

|
| Vitiligo-Repeats |

|
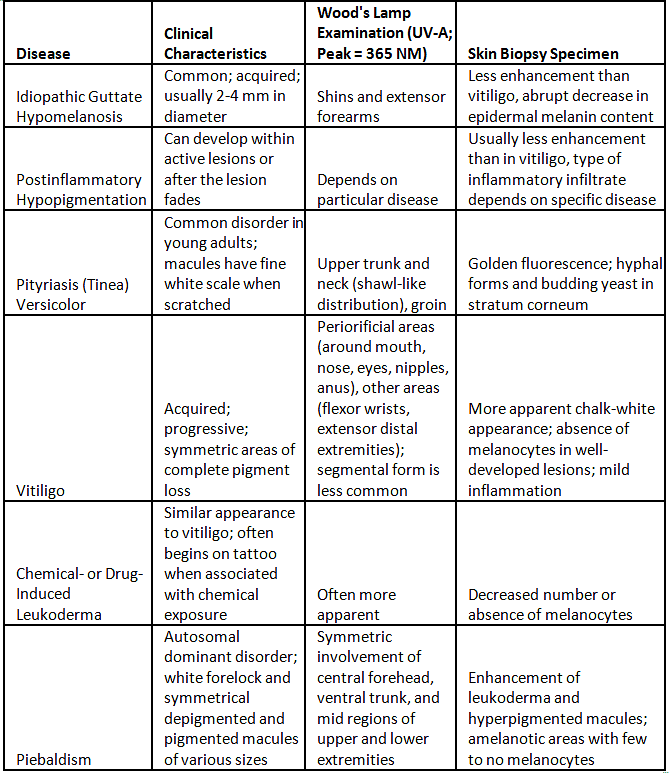
Hypo pigmented patches-Differential diagnosis
I. Primary Cutaneous Disorders
A. Diffuse
- Generalized vitiligo
B. Localized
- Idiopathic guttate hypomelanosis
- Postinflammatory
- Tinea (pityriasis) versicolor
- Vitiligo
- Chemical- or drug-induced leukoderma
- Nevus depigmentosus
- Piebaldism
II. Systemic Diseases
A. Diffuse
- Oculocutaneous albinism
- Hermansky-Pudlak syndrome
- Chediak-Higashi syndrome
- Phenylketonuria
B. Localized
- Systemic sclerosis (scleroderma)
- Melanoma-associated leukoderma
- Vogt-Koyanagi-Harada syndrome
- Onchocerciasis
- Sarcoidosis
- Cutaneous T cell lymphoma (especially mycosis fungoides)
- Tuberculoid and indeterminate leprosy
- Linear nevoid hypopigmentation (hypomelanosis of Ito)
- Incontinentia pigmenti (stage IV)
- Tuberous sclerosis
- Waardenburg syndrome
Vitiligo-Etiology
- Uncertain Etiology: The precise cause of Vitiligo remains unidentified.
- Multifactorial Nature: Vitiligo is suggested to be a multifactorial condition, involving a combination of genetic susceptibility and environmental factors.
- Genetic and Environmental Factors: Both genetic predisposition and environmental influences are believed to contribute to the development of Vitiligo.
- Risk Factors:
- Family History: Individuals with a family history of Vitiligo are at an increased risk.
- Autoimmune Diseases: Risk is associated with other autoimmune disorders like Hashimoto's thyroiditis, scleroderma, rheumatoid arthritis, type 1 diabetes mellitus, psoriasis, Addison's disease, pernicious anemia, alopecia areata, systemic lupus erythematosus, hypothyroidism, and celiac disease.
Vitiligo-Etiology (Theories)
- Unknown Cause: Despite various proposed theories, the exact cause of vitiligo remains unknown.
- Agreed Principles:
- Functional loss of melanocytes.
- Histochemically recognized melanocytes may be absent.
- Destruction, likely gradual, leading to a decrease in melanocytes.
- Theories on Destruction:
- Autoimmune Mechanism: Supported by evidence of circulating antibodies against melanocyte proteins in vitiligo patients. This theory suggests alterations in humoral and cellular immunity leading to melanocyte destruction, especially in nonsegmental vitiligo associated with autoimmune conditions.
- Cytotoxic Mechanism: Involves melanocyte dysfunction or destruction due to immune surveillance.
- Intrinsic Melanocyte Defects: Proposes inherent abnormalities in melanocytes hindering their growth and differentiation in conditions supportive of normal melanocytes.
- Oxidant-Antioxidant Mechanisms: Suggests that a metabolic product of melanin synthesis may cause melanocyte destruction.
- Neural Hypothesis: Involves a neurochemical mediator that destroys melanocytes or inhibits melanin production.
- Association with Autoimmune Conditions: Vitiligo, especially nonsegmental vitiligo, is often linked to autoimmune disorders such as Hashimoto thyroiditis, Graves disease, Addison disease, diabetes mellitus, alopecia areata, pernicious anemia, inflammatory bowel disease, psoriasis, and autoimmune polyglandular syndrome.
- Composite Hypothesis: Since none of the individual theories is entirely satisfactory, some suggest a composite hypothesis that combines elements from different theories.
Vitiligo-Presentation
- Distinctive Features:
- Lesions exhibit depigmented papules.
- Margins are sharply outlined and may merge to create geographical patterns.
- Hair in affected areas can lose pigmentation (known as leukotrichia).
- Distribution of lesions is widespread, with a higher susceptibility in trauma-prone regions.
- Lesion Characteristics:
- Lesions can manifest anywhere on the body.
- The progression of the condition is typically slow, although in some cases, it may advance rapidly.
- The presence of Koebner phenomenon is noted, indicating the development of lesions at sites of skin trauma.
Clinical Classification
Vitiligo is categorized into two main groups: segmental and non-segmental. The differentiation between these two groups holds significant clinical relevance, influencing considerations related to progression, prognosis, and therapeutic approaches.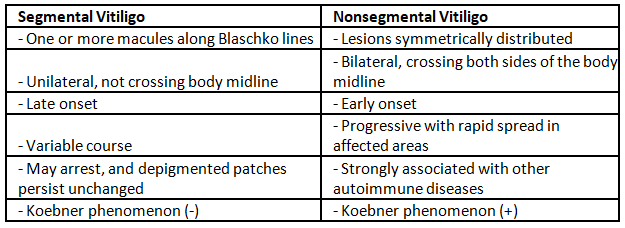
 |
Download the notes
Vitiligo
|
Download as PDF |
Vitiligo-Diagnosis
Diagnosis of Vitiligo
- Lesions become more apparent and look chalky white under a Wood's lamp.
- Microscopic examination shows a complete loss of epidermal pigmentation, indicating a cell-mediated process destroying melanocytes in the epidermis.
- Immunohistochemistry testing may be performed to assess melanocytes, and laboratory work may include a thyroid panel, antinuclear antibody, and antithyroid peroxidase antibody.
- Assessment of extent and severity of vitiligo involves a numerical score system based on the rule of nines, evaluating five sites affected (head, upper limbs, trunk, lower limbs, and genitalia) using five stages of disease intensity.
- The VETI score is calculated based on the percentage of involvement and the grade of intensity for each site, providing a constant and reproducible measure. The maximum VETI score is 55.5.
Treatment of Vitiligo
- Localized Disease
- New Lesions: Topical steroids, topical calcineurin inhibitors
- Old Lesions: Topical PUV A/P U V A plus UVA
- Extensive Disease
- New Lesions (Rapid Increase): Oral steroids, PUVA, narrow band UVB
- Old Lesions: Oral steroids, PUVA, narrow band UVB
- Intolerance to PUVA: Oral steroids
- Sunscreen, topical tacrolimus, and camouflage makeup are recommended for cosmetic reasons.
- New Therapies
- Afamelanotide: A long-lasting synthetic analog of alpha-melanocyte-stimulating hormone, which stimulates melanocyte proliferation and melanogenesis.
- Depigmentation: In carefully selected patients, a 20% cream of monobenzyl ether of hydroquinone is applied twice daily for 3-12 months.
- Refractory Patients
- Surgical Techniques: Punch grafting, split skin grafting, blister grafting, and melanocyte transfer can be considered for refractory but stable patients.
Vitiligo-Repeats
Q1: Mention various causes of hypo pigmented lesions of skin. Give a brief account of any two of such lesions. (2002)
Q2: Discuss Etiopathogenesis of Vitiligo. (2009)
Q3: What are various etiological factors for causation of Vitiligo? Enumerate various disorders associated with Vitiligo. (2013)
Q4: A 25-year-old unmarried female presents with asymptomatic depigmented macules of varying sizes over the breast, back, arms and legs for the last two years (2015)
i. List the different diagnosis.
ii. How would you investigate this patient?
iii. How would you treat the most common condition manifesting with the given symptomatology?
Q5: Describe various theories which have been proposed to explain the pathogenesis of vitiligo. How do you assess the severity of vitiligo? Describe the lines of treatment of various grades of the disease. (2018)
|
7 videos|219 docs
|
FAQs on Vitiligo - Medical Science Optional Notes for UPSC
| 1. What are the possible causes of hypo-pigmented patches on the skin? |  |
| 2. What is the most common cause of hypo-pigmented patches known as vitiligo? |  |
| 3. What are the theories regarding the etiology of vitiligo? |  |
| 4. How is vitiligo clinically classified? |  |
| 5. How is vitiligo diagnosed? |  |