Human Reproduction Chapter Notes | Biology Class 12 - NEET PDF Download
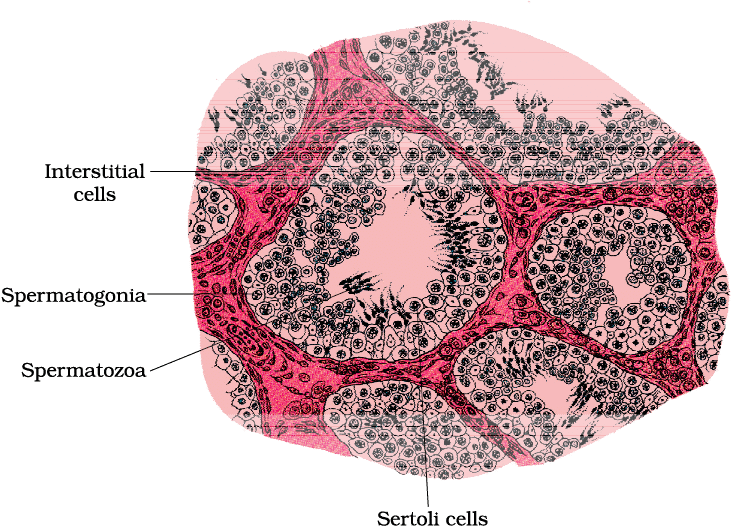
Reproduction, one of the most fundamental aspects of life, is a fascinating process in humans. It involves the formation of sperm in males and ova in females, the transfer of sperm into the female genital tract, the fusion of gametes, the attachment of the fertilised egg to the uterine wall, and the development of the embryo.
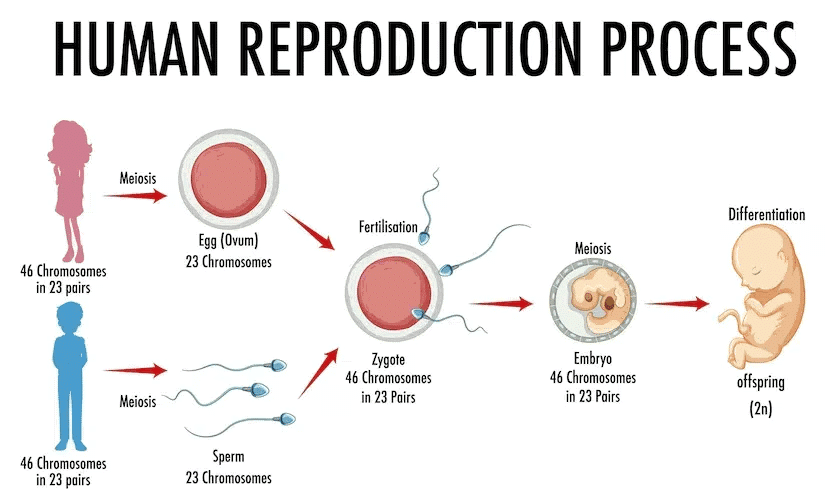
Male Reproductive System
The male reproductive system is located in the pelvis region.
There are four main parts in the male reproductive system:
- Testes
- Accessory ducts
- Glands
- External Genitalia
(a) Testes
- The testes are situated outside the abdominal cavity within a pouch called the scrotum.
- The scrotum helps keep the temperature lower, about 2-2.5°C cooler than the body's internal temperature. This is important for spermatogenesis, which is the process of making sperm.
- Each testis is oval in shape, approximately 4 to 5 cm long and 2 to 3 cm wide in adults.
- Inside each testis, there are around 250 compartments known as testicular lobules.
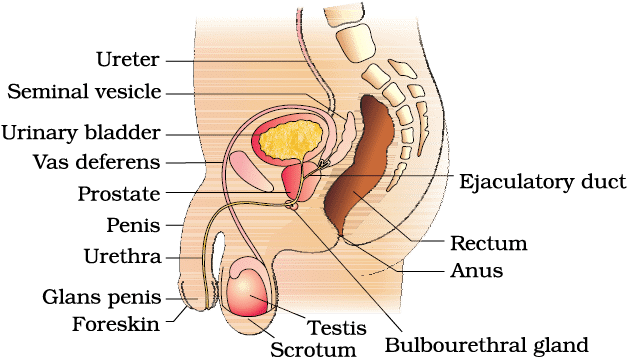
Seminiferous Tubules and Spermatogenesis
The testis is made up of many small compartments called lobules. Each lobule contains seminiferous tubules, which are tightly coiled structures where sperm are produced. These tubules are lined with two types of cells:
(i) Male germ cells (spermatogonia): These cells divide through a process called meiosis, eventually leading to the formation of sperm.
(ii) Sertoli cells: These cells provide essential nutrients and support to the germ cells during the process of sperm production.
Interstitial Spaces or Leydig Cells
- The areas outside the seminiferous tubules, known as interstitial spaces, are filled with small blood vessels and special cells called Leydig cells.
- Leydig cells are responsible for producing and releasing male hormones known as androgens.
- These interstitial spaces also contain other important immune cells that help the body fight infection
(b) Male Accessory Ducts
The accessory ducts facilitate the transportation of the sperm from the testes to the urethra for their release outside the body. The male reproductive system consists of four accessory ducts:
- Rete Testis
- Vasa efferentia
- Epididymis
- Vas deferens
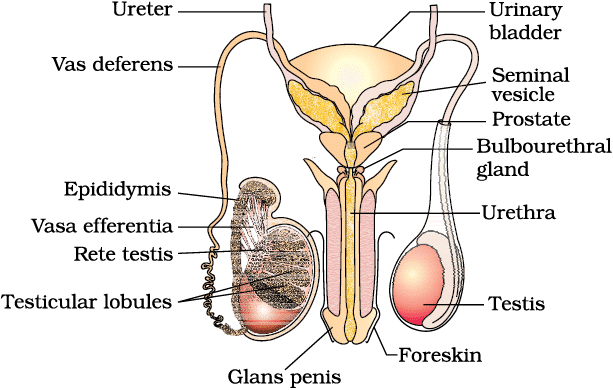
- Sperm is produced in the seminiferous tubules of the testis and then transported through a series of structures.
- Sperm travels from the seminiferous tubules to the vasa efferentia via the rete testis.
- The vasa efferentia carry sperm from the testis to the epididymis, which is located along the back of each testis.
- In the epididymis, sperm mature and are stored until ejaculation.
- From the epididymis, sperm move into the vas deferens, which ascends into the abdomen and loops over the urinary bladder.
- The vas deferens joins with a duct from the seminal vesicle to form the ejaculatory duct.
- The ejaculatory duct opens into the urethra, which carries sperm out of the body.
- The urethra originates from the urinary bladder and extends through the penis, ending at the urethral meatus, the external opening.
(c) Male Accessory Glands
The male accessory glands include paired seminal vesicles, a prostate, and paired bulbourethral glands.
- Seminal Vesicles: These are paired glands that contribute to the formation of seminal plasma.
- Prostate Gland: This gland adds to the seminal fluid and plays a crucial role in reproduction.
- Bulbourethral Glands: These paired glands help in lubricating the penis and also contribute to the seminal fluid.
Functions of Secretions:
- The secretions from these glands are rich in fructose, which provides energy for sperm.
- They also contain calcium and various enzymes that are important for sperm function and mobility.
- The secretions from the bulbourethral glands also aid in the lubrication of the penis, facilitating sexual intercourse.
(d) External Genitalia
- The penis is the male external reproductive organ. It consists of specialized tissue that enables erection, which is essential for insemination.
- The tip of the penis, known as the glans penis, is covered by a loose fold of skin called the foreskin.
Female Reproductive System
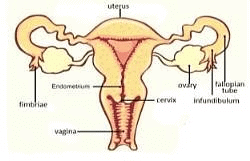
The female reproductive system includes a pair of ovaries, a pair of oviducts, the uterus, the cervix, the vagina, and the external genitalia, all located in the pelvic region.
These parts work together both structurally and functionally. The system is essential for several important processes:
- Ovulation: the release of eggs from the ovaries.
- Fertilisation: when a sperm joins an egg.
- Pregnancy: the time when a fertilised egg develops in the uterus.
- Birth: the process of delivering a baby.
- Child care: taking care of a newborn after birth.
Additionally, the system includes a pair of mammary glands that are also important for nurturing the baby.

(a) Ovaries
The primary female sex organs that produce the ovum and several ovarian hormones, steroid in nature.
- Located one on each side of the lower abdomen.
- Each ovary is covered by a thin epithelium which encloses the ovarian stroma.
- The ovarian stroma is divided into two zones – a peripheral cortex and an inner medulla.
(b) Oviduct (fallopian tube)
- 10-12 cm in length.
- Extends from the periphery of each ovary to the uterus.
- The part closer to the ovary is the funnel-shaped infundibulum.
- Fimbriae are the finger-like projections located on the edges of the infundibulum.
- Fimbriae help in the collection of the ovum after ovulation.
- The infundibulum leads to the ampulla, which is the wider part of the oviduct.
- The last part of the oviduct isthe isthmus which has a narrow lumen and it joins the uterus.
(c) Uterus
- Uterus is also called womb.
- The shape of the uterus is like an inverted pear.
- Ligaments attached to the pelvic wall support the uterus.
- The narrow cervix opens the uterus into the vagina.
- Cervical canal is the cavity of the cervix which forms birthcanal along with vagina.
- Three layers of tissues are present in the uterus wall- the outer thin membrane bound perimetrium, middle thick layer of smooth muscle called myometrium, inner glandular layer called endometrium.
- Endometrium lines the uterine cavity.
- During menstrual cycle, endometrium undergoes cyclical changes but the myometrium exhibits strong contraction during parturition.
(d) External Genitalia

- Vagina is the female external genitalia.
- Vagina includes mons pubis, labia majora (labia majus), labia minora (labia minora), hymen and clitoris.
- Mons pubis is a cushion of fatty tissue covered by skin and pubic hair.
- The labia majora are folds of tissue extend down from the mons pubis and surround the vaginal opening.
- Under the labia majora, there are paired tissue folded to form labia minora.
- Hymen is membrane covering the opening of the vagina.
- A tiny finger-like structure which lies at the upper junction of the two labia minora above the urethral opening is called clitoris.
Mammary Glands
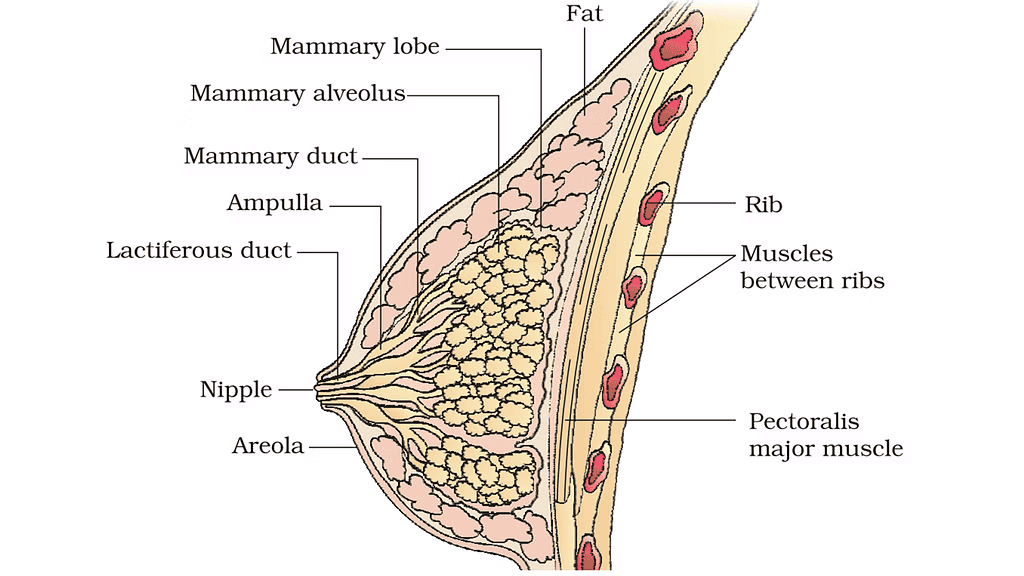 A diagrammatic sectional view of Mammary gland
A diagrammatic sectional view of Mammary gland
- Paired structures containing glandular tissues and fats, the amount of fat varies from person to person.
- The glandular tissue of each breast is divided into 15-20 mammary lobes containing clusters of cells called alveoli.
- The cells of alveoli secrete milk, which is stored in the cavities called as lumens of alveoli.
- The alveoli open into mammary tubules and the tubules of each lobe join to form a mammary duct which joins to form a wider mammary ampulla.
- Mammary ampulla is connected to lactiferous duct through which milk is sucked out.
Gametogenesis
The process of formation of gametes in primary sex organs( the testis in the males and the ovaries in the females) is called Gametogenesis.
Gametogenesis includes
(a) Spermatogenesis and Spermiogenesis in males
(b) Oogenesis in females.
(a) Spermatogenesis and Spermiogenesis

- Immature male germ cells in the testis, known as spermatogonia,produce sperm through a process called spermatogenesis,which begins at puberty.
- Spermatogonia,which are diploid cells with 46 chromosomes, multiply by mitotic division and increase in number. Some of these cells develop into primary spermatocytes,which undergo meiosis.
- A primary spermatocyte undergoes the first meiotic division,known as reduction division, producing two haploid cells called secondary spermatocytes, each containing 23 chromosomes.
- The secondary spermatocytes then undergo the second meiotic division, leading to the formation of four haploid spermatids.
- The spermatids undergo a transformation process called spermiogenesis to become mature sperm cells, sperm heads become embedded in Sertoli cells and are eventually released from the seminiferous tubules through a process called spermiation.

Hormonal control of spermatogenesis
Initiation at Puberty: Spermatogenesis begins at puberty due to an increase in the secretion of gonadotropin-releasing hormone (GnRH) from the hypothalamus.
- Role of GnRH: The increased GnRH stimulates the anterior pituitary gland to secrete two gonadotropins: luteinizing hormone (LH) and follicle-stimulating hormone (FSH).
- Action of LH: LH acts on Leydig cells in the testes, stimulating the synthesis and secretion of androgens (male hormones).
- Role of Androgens: Androgens promote spermatogenesis, the process of sperm production.
- Action of FSH: FSH acts on Sertoli cells in the testes, stimulating the secretion of factors that aid in spermiogenesis, the final stage of sperm development.

Structure of a Sperm

- Sperm are made up of a head, neck, middle piece, and tail.
- The entire sperm is covered by a plasma membrane.
- Head: Contains a haploid nucleus. The acrosome, a cap-like structure filled with enzymes that aid in fertilization, covers the front part of the nucleus.
- Middle Piece: Packed with mitochondria that provide energy for the tail's movement.
- Tail: Facilitates sperm motility, which is crucial for fertilization.
- During ejaculation, a human male releases about 200 to 300 million sperm. For normal fertility: At least 60% of sperm must have a normal shape and size and At least 40% must show vigorous motility.
- Sperm produced in the seminiferous tubules are transported by accessory ducts.
- Secretions from the epididymis, vas deferens, seminal vesicle, and prostate are necessary for sperm maturation and motility.
- Semen is composed of seminal plasma and sperm.
- The function of male sex accessory ducts and glands is regulated by testicular hormones (androgens).
(b) Oogenesis
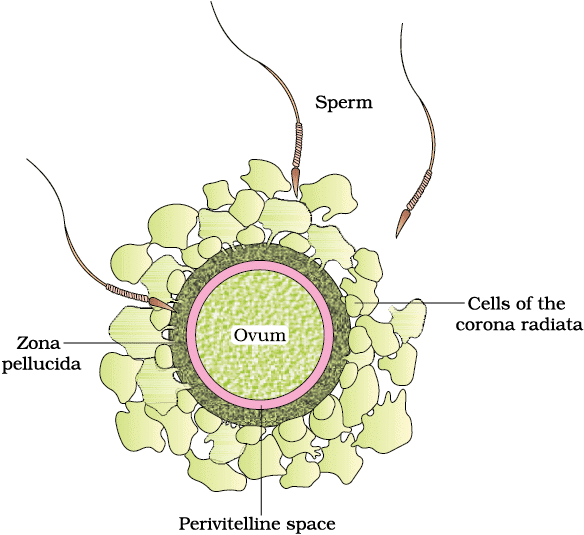
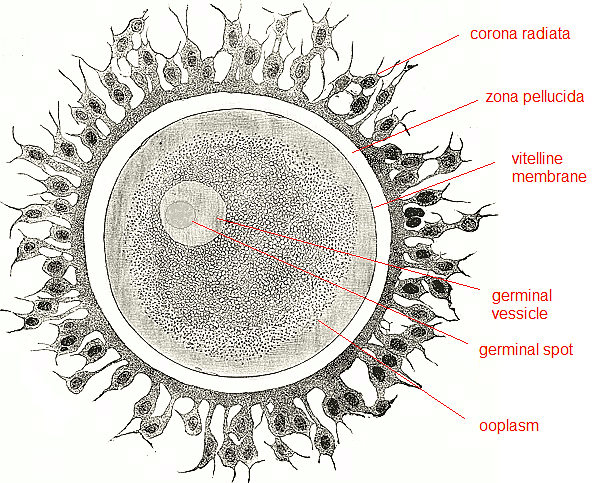 Structure of Human Ovum
Structure of Human Ovum
- Oogenesis is the process of forming a mature female gamete, and it is quite different from spermatogenesis.
- It begins during embryonic development when millions of gamete mother cells, called oogonia, are formed in each fetal ovary. After birth, no more oogonia are produced.
- These cells start dividing and enter prophase-I of meiotic division, getting temporarily arrested at this stage. They are then called primary oocytes.

- Each primary oocyte is surrounded by a layer of granulosa cells, forming a primary follicle. A large number of these follicles degenerate from birth to puberty, leaving only 60,000-80,000 primary follicles in each ovary at puberty.
- At puberty, primary follicles develop into secondary follicles, with more layers of granulosa cells and a new theca layer.
- The secondary follicle soon becomes a tertiary follicle, characterized by a fluid-filled cavity called the antrum. The theca layer is organized into an inner theca interna and an outer theca externa.
- During this stage, the primary oocyte within the tertiary follicle grows in size and completes its first meiotic division. This division is unequal, resulting in a large haploid secondary oocyte and a tiny first polar body. The secondary oocyte retains most of the nutrient-rich cytoplasm.
- The first polar body may either divide further or degenerate, but this is not yet certain.
- The tertiary follicle continues to mature into a Graafian follicle, where the secondary oocyte is surrounded by a new membrane called the zona pellucida.
- The Graafian follicle eventually ruptures, releasing the secondary oocyte (ovum) from the ovary in a process called ovulation.
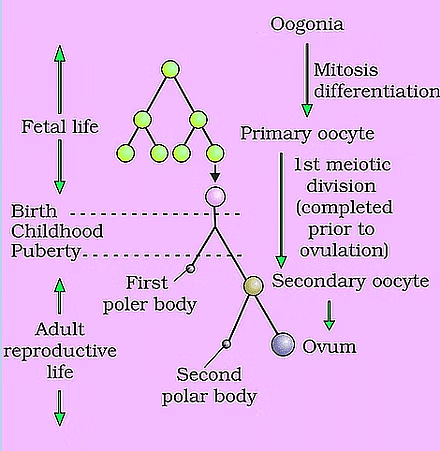 Oogenesis
Oogenesis
Menstrual Cycle
In female primates like monkeys, apes, and humans, the reproductive cycle is known as the menstrual cycle. Menarche is the term used for the first menstruation, which occurs at puberty. In human females, menstruation typically occurs every 28 to 29 days, marking the beginning of a new menstrual cycle. During each menstrual cycle, an egg (or ovum) is released from the ovary in a process called ovulation.
Phases of Menstrual Cycle
1. Menstrual Phase
- The menstrual cycle consists of several phases, starting with the menstrual phase. This phase lasts for about 3 to 5 days and involves the shedding of the uterine lining, which is expelled through the vagina. This occurs when the released ovum is not fertilized.
- If fertilization does not take place, menstruation occurs. A missed period can indicate pregnancy, but it can also result from factors like stress or poor health.
2. Follicular Phase
- After the menstrual phase, the cycle enters the follicular phase, during which primary follicles in the ovary mature into a Graafian follicle, and the uterine lining (endometrium) begins to regenerate.
- The growth and maturation of the follicles and the regeneration of the endometrium are regulated by changes in the levels of hormones from the pituitary gland and the ovaries.
- During the follicular phase, the levels of pituitary hormones luteinizing hormone (LH) and follicle-stimulating hormone (FSH) increase, promoting follicular development and the secretion of estrogen by the growing follicles.
3. Ovulatory Phase
- LH and FSH peak around the middle of the cycle, typically around the 14th day.
- A rapid increase in LH, known as the LH surge, triggers the rupture of the Graafian follicle and the release of the ovum, marking the ovulatory phase.
4. Luteal Phase
- Following ovulation, the cycle enters the luteal phase, during which the remnants of the Graafian follicle transform into the corpus luteum.
- The corpus luteum secretes large amounts of progesterone, which is crucial for maintaining the endometrium. A healthy endometrium is necessary for the implantation of a fertilized egg and the subsequent stages of pregnancy.

During pregnancy, the events of the menstrual cycle are halted, and menstruation does not occur. If fertilization does not happen, the corpus luteum degenerates, leading to the breakdown of the endometrium and the onset of menstruation, signaling the start of a new cycle. In human females, menstrual cycles typically cease around the age of 50, a process known as menopause. Cyclic menstruation is a sign of a normal reproductive phase, which spans from menarche to menopause.
Fertilization
- During copulation, semen is released into the vagina, where motile sperm swim rapidly through the cervix and into the uterus, eventually reaching the ampullary region of the fallopian tube.
- Simultaneously, the ovum is transported from the ovary to the same region, where fertilization occurs.
- Fertilization can only happen if both the ovum and sperm reach the ampullary region at the same time, which is why not all instances of copulation result in fertilization and pregnancy.
- The fusion of a sperm with an ovum is known as fertilization.
- When a sperm contacts the zona pellucida layer of the ovum, it triggers changes in the membrane that prevent additional sperm from entering.
- This ensures that only one sperm can fertilize an ovum.
- The acrosome's secretions help the sperm penetrate the ovum's cytoplasm through the zona pellucida and plasma membrane, completing the meiotic division of the secondary oocyte.
- The second meiotic division is unequal, resulting in a second polar body and a haploid ovum (ootid).
- The haploid nuclei of the sperm and ovum then fuse to form a diploid zygote.
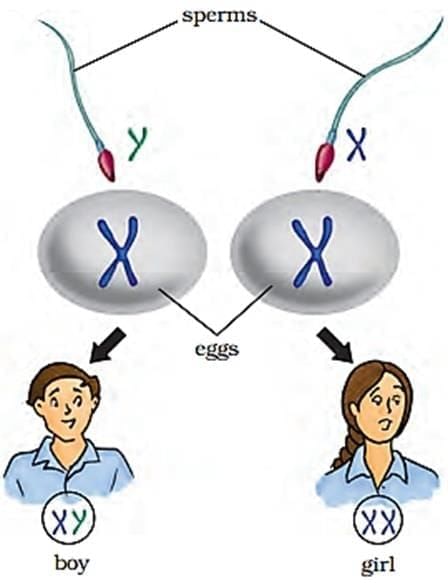
Determining Chromosome Number and Sex of the Baby
- The zygote's chromosome number is determined by the fusion of the haploid nuclei from the sperm and ovum.
- The sex of the baby is also determined at this stage.
- Human females have XX chromosomes, while males have XY.
- Female gametes (ova) always carry an X chromosome, while male gametes (sperms) carry either an X or a Y chromosome.
- As a result, 50% of sperms carry an X chromosome and 50% carry a Y chromosome.
- When the sperm fertilizes the ovum, the zygote will have either XX (female) or XY (male) chromosomes.
- If the sperm carrying X fertilizes the ovum, the zygote will be XX and develop into a female baby.
- If the sperm carrying Y fertilizes the ovum, the zygote will be XY and develop into a male baby.
- This is why it is scientifically accurate to say that the sex of the baby is determined by the father, not the mother.
Cleavage and Early Development
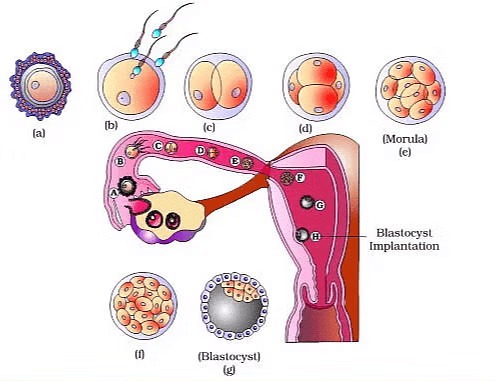 Transport of ovum, fertilisation and passage of growing embryo through fallopian tube
Transport of ovum, fertilisation and passage of growing embryo through fallopian tube
- As the zygote moves through the isthmus of the oviduct toward the uterus, mitotic division begins, resulting in the formation of 2, 4, 8, and 16 daughter cells called blastomeres.
- An embryo with 8 to 16 blastomeres is known as a morula. The morula continues to divide and transforms into a blastocyst as it moves further into the uterus.
- In the blastocyst, the blastomeres are arranged into an outer layer called trophoblast and an inner group of cells called the inner cell mass. The trophoblast layer attaches to the endometrium, and the inner cell mass differentiates into the embryo.
Implantation and Pregnancy
- After attachment, the uterine cells divide rapidly, covering the blastocyst. This process, called implantation, leads to pregnancy as the blastocyst becomes embedded in the endometrium of the uterus.
Pregnancy and Embryonic Development
- After implantation, finger-like projections called chorionic villi emerge from the trophoblast.
- These chorionic villi, surrounded by uterine tissue and maternal blood, interdigitate with the uterine tissue, forming a structural and functional unit known as the placenta.
- This unit is crucial for the developing embryo (fetus) as it facilitates the exchange of essential substances between the mother and the embryo.
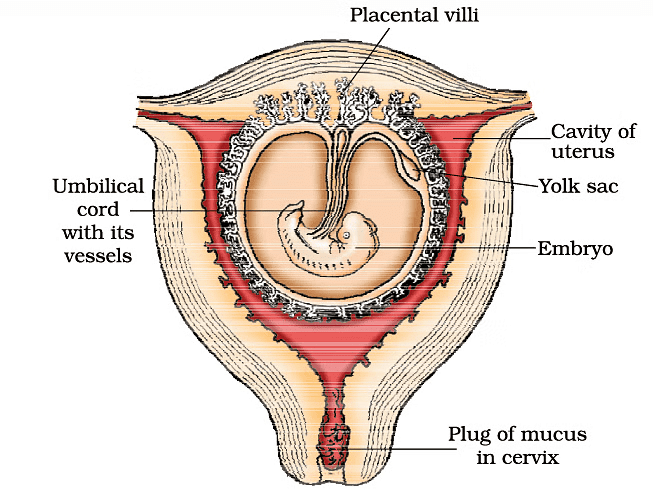 The human foetus within the uterus
The human foetus within the uterus
Functions of the placenta
- Oxygen and Nutrient Supply: The placenta is responsible for providing the developing embryo with oxygen and essential nutrients necessary for growth and development.
- Waste Removal: It also plays a vital role in removing waste products such as carbon dioxide and other excretory materials produced by the embryo.
- Hormone Production: The placenta acts as an endocrine organ, producing several important hormones, including:
- human chorionic gonadotropin (hCG), which helps maintain pregnancy;
- human placental lactogen (hPL), which regulates metabolism;
- estrogens and progestogens, which support pregnancy.
- Umbilical Cord: The placenta is connected to the embryo via the umbilical cord, which facilitates the transport of substances to and from the embryo.
- Hormonal Changes During Pregnancy: During pregnancy, there is an increase in the levels of various hormones in the maternal blood, such as cortisol, prolactin, and thyroxine. These hormonal changes are crucial for supporting fetal growth, metabolic adjustments in the mother, and maintaining the pregnancy.
Early Embryonic Development
Shortly after implantation, the inner cell mass of the embryo differentiates into three germ layers:
- Ectoderm: The outer layer, which will develop into various tissues, including the skin and nervous system.
- Endoderm: The inner layer, which will give rise to internal organs such as the digestive system and respiratory system.
- Mesoderm: The middle layer, which will develop into muscles, bones, and the circulatory system.
The inner cell mass contains stem cells, which have the potential to differentiate into any type of tissue or organ in the body. This ability is crucial for the proper development of the embryo into a fully formed organism.
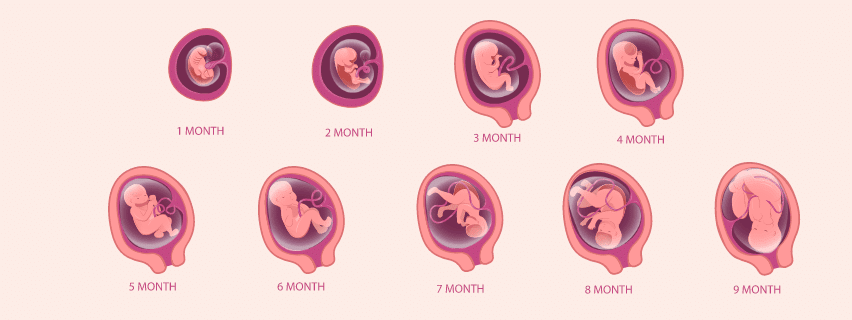
Features of Embryonic Development at Various Months of Pregnancy
- Human Pregnancy: Lasts for 9 months.
- In human beings, after one month of pregnancy, the heart of the embryo starts to form.
- The first indication of the developing fetus can be detected by carefully listening to its heart sounds using a stethoscope.
- By the end of the second month of pregnancy, the fetus begins to develop limbs and digits.
- At the end of twelve weeks (the end of the first trimester), most major organ systems are formed, including well-developed limbs and external genital organs.
- The first movements of the fetus and the appearance of hair on its head are typically noticed during the fifth month.
- By about twenty-four weeks (the end of the second trimester), the body is covered with fine hair, the eyelids are separating, and eyelashes have formed.
- By the end of nine months of pregnancy, the fetus is fully developed and ready for delivery.
Parturition and Lactation
The average duration of human pregnancy is about 9 months, known as the gestation period. At the end of this period, vigorous contractions of the uterus lead to the expulsion and delivery of the fetus. This process, called parturition, is triggered by a complex neuroendocrine mechanism.
Parturition
Parturition is the process of childbirth, where the baby is expelled from the uterus through the birth canal.
- Parturition is initiated by a complex neuroendocrine mechanism involving signals from the fully developed fetus and the placenta. These signals induce mild uterine contractions known as the fetal ejection reflex.
- Oxytocin, a hormone released from the maternal pituitary gland, plays a crucial role in parturition.
- It acts on the uterine muscles, causing stronger contractions.
- The release of oxytocin stimulates further uterine contractions, creating a positive feedback loop.
- The process of parturition involves a series of increasingly strong uterine contractions.
- These contractions continue to intensify, leading to the expulsion of the baby through the birth canal.
- Immediately after the infant is delivered, the placenta is also expelled from the uterus.
Lactation
Lactation is the process by which the mammary glands of the mother produce milk to feed the newborn.
- During pregnancy, the mammary glands undergo differentiation and prepare to produce milk.
- Milk production typically begins towards the end of pregnancy.
- The milk produced in the initial days of lactation is called colostrum.
- Colostrum is rich in antibodies that are crucial for developing the newborn's immune resistance.
- Doctors recommend breastfeeding during the early period of infant growth.
- Breastfeeding helps ensure the healthy development of the baby.
Add Content FAQs
Add Questions
Add QuestionAnswer: B Solution: During spermatogenesis, male germ cells or spermatogonia differentiate into diploid primary spermatocytes. These primary spermatocytes then undergo meiosis I to produce haploid secondary spermatocytes. The secondary spermatocytes further undergo meiosis II to produce four haploid spermatids, which then differentiate into spermatozoa. QuestionId: 775593 Difficulty Level: Easy Total Attempted: 0 |
Q. 776155 Show At : 0 seconds What is the function of the scrotum in the male reproductive system? Answer: D Solution:
QuestionId: 776155 Difficulty Level: Easy Total Attempted: 0 |
Q. 776156 Show At : 0 seconds What is the function of the accessory ducts in the male reproductive system? Answer: C Solution:
Therefore, the correct answer is (c) To transport sperm from the testes to the urethra. QuestionId: 776156 Difficulty Level: Easy Total Attempted: 0 |
Q. 776157 Show At : 0 seconds Which of the following statements about the prostate gland is true? Answer: B Solution:
Therefore, the statement "It aids in the survival of sperm in an acidic environment" is true. QuestionId: 776157 Difficulty Level: Easy Total Attempted: 0 Reported Count: 1 |
775593,776155,776156,776157
|
59 videos|290 docs|168 tests
|