First trimester bleeding | Medical Science Optional Notes for UPSC PDF Download
Abdominal pain during pregnancy-DIFFERENTIAL DIAGNOSIS
Every woman with an early pregnancy, vaginal bleeding, and pain should be evaluated. The primary goal is prompt diagnosis of an ectopic pregnancy. Serial quantitative serum β-hCG and progesterone levels and transvaginal sonography are used to ascertain if there is an intrauterine live fetus. Because these are not 100-percent accurate to confirm early fetal death or location, repeat evaluations are often necessary.
The differential diagnosis for abdominal pain coexistent with pregnancy is extensive.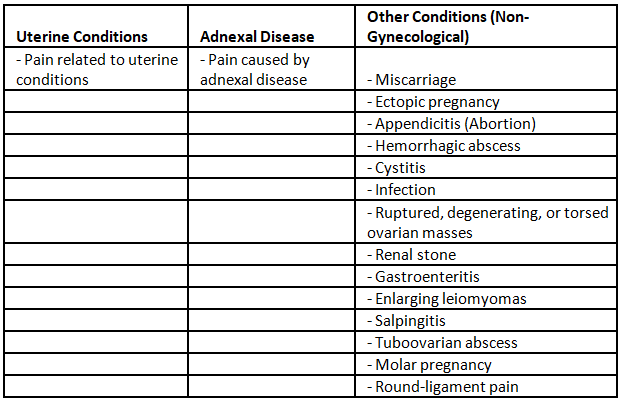
Abortion, Ectopic pregnancy and Molar pregnancy are associated with vaginal bleeding.
Differential diagnosis
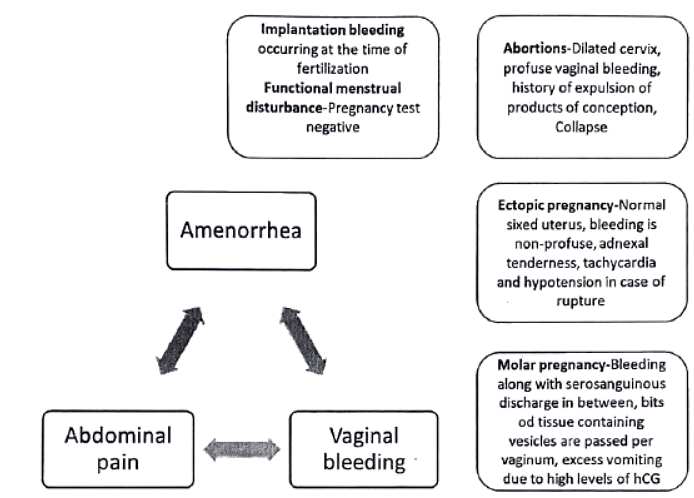
First trimester bleeding
Pre-existing or Exacerbated During Pregnancy:
- Cervico-vaginitis
- Vascular erosion
- Cervical polyp
- Uterine fibroid
- Ruptured varicose veins
- Malignancy
- Trauma
- Drugs (Anticoagulants, Antiepileptics)
- Coagulopathy
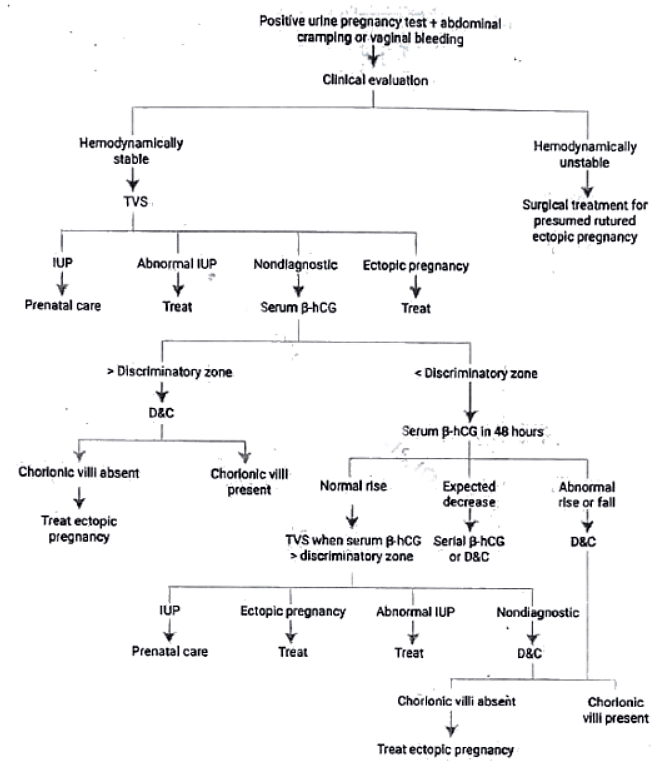
Management protocol
- Diagnostic Process for Bleeding or Pain with Positive Pregnancy Test:
- Initial Trans Vaginal Ultrasound (TVS) commonly performed to locate gestation.
- Identification of Yolk Sac, Embryo, or Fetus:
- If any of these are identified within the uterus or adnexa, a diagnosis can be established.
- Abnormal Intrauterine Pregnancy (IUP) - Hydatidiform Mole:
- In the case of abnormal IUP with a snowstorm appearance and absent fetal parts (hydatidiform mole), appropriate treatment is administered.
- Non-Diagnostic Scenario - Evaluate Serum Beta hCG:
- If there is an absence of fetal parts in both the uterus and adnexa, it is considered non-diagnostic.
- Serum Beta hCG evaluation is recommended in such cases.
- Discriminatory Zone for Serum Beta hCG:
- Investigators have defined a discriminatory zone, i.e., a serum 3-hCG concentration above which failure to visualize an intrauterine pregnancy indicates a nonviable or ectopic pregnancy.
- Barnhart et al. (1994) found that an empty uterus with a serum 3-hCG concentration > 1500 mlU/mL was 100 percent accurate in excluding a live uterine pregnancy.
Ectopic Pregnancy
Risk factors
- Congenital anomalies of fallopian tubes
- Prior tubal surgery
- Prior PID
- Use of IUCD
- Use of progestogen contraceptives
- Assisted reproductive technologies
- Previous tubal pregnancies
Options for ectopic tubal pregnancy treatment include medical (single dose or multi dose methotrexate therapy) and surgical (laparoscopic salpingostomy) approaches.
Medical vs Surgical approach
- Women treated with methotrexate had significantly better physical functioning immediately following therapy, but there were no differences in psychological functioning.
- Ectopic resolution success rates were not significantly different between those managed surgically and those treated with methotrexate.
Conclusion from various studies-Women who are hemodynamically stable and in whom there is a small tubal diameter, no fetal cardiac activity, and serum (S-hCG concentrations < 5000 mlU/mL have similar outcomes with medical or surgical management. Despite lower success rates with medical therapy for women with larger tubal size, higher serum (3-hCG levels, and fetal cardiac activity, medical management can be offered to the motivated woman who understands the risks.
Role of expectant management in Ectopic pregnancy
- Indication: Very early tubal pregnancies associated with stable or decreasing serum β-hCG levels.
- Statistics from the American College of Obstetricians and Gynecologists (2012): 88 percent of ectopic pregnancies resolve when β-hCG levels are below 200 mlU/mL.
- Expectant Management Comparative to Surgery and Medical Approaches: Subsequent rates of tubal patency and intrauterine pregnancy are similar with expectant management, surgery, and medical interventions.
- Considerations for Expectant Therapy: The potential serious consequences of tubal rupture, along with the known safety of medical and surgical treatments, emphasize that expectant therapy should be pursued only in appropriately selected and counseled women.
Medical treatment protocol for ectopic pregnancy
Methotrexate is highly effective against rapidly proliferating tissue such as trophoblast, and overall ectopic tubal pregnancy resolution rates approximate 90 percent with its use.
For ease and efficacy, intramuscular methotrexate administration is used most frequently for ectopic pregnancy resolution, and single-dose and multi dose methotrexate protocols are available.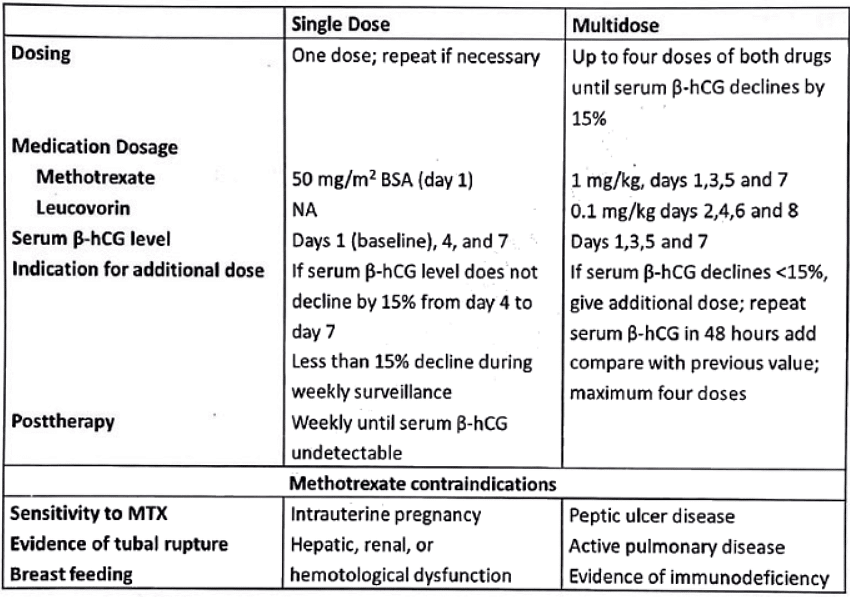 Single-dose therapy offers simplicity, less expense, and less intensive post therapy monitoring and does not require leucovorin rescue. Higher success rate for the multi-dose regimen is reported in most of the studies.
Single-dose therapy offers simplicity, less expense, and less intensive post therapy monitoring and does not require leucovorin rescue. Higher success rate for the multi-dose regimen is reported in most of the studies.
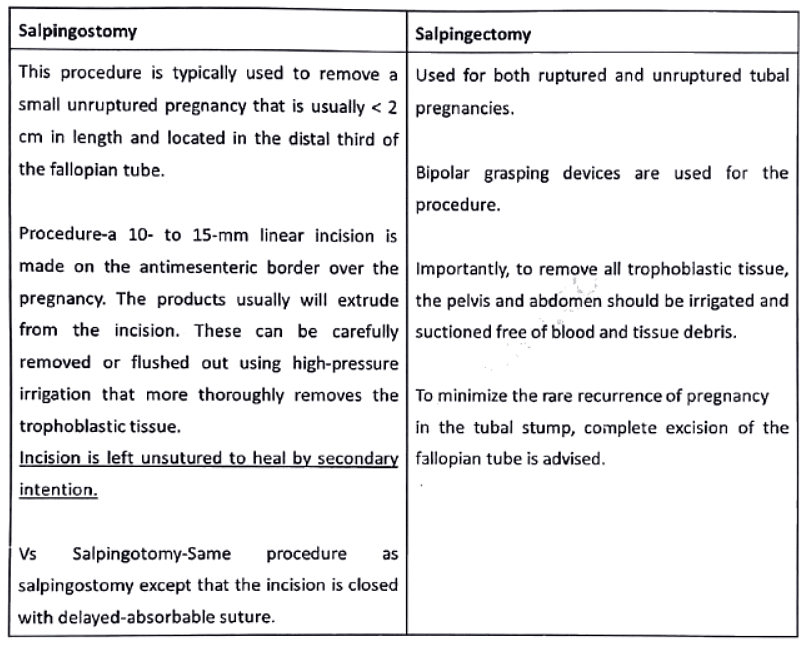
Surgical management for ectopic tubal pregnancy
 |
Download the notes
First trimester bleeding
|
Download as PDF |
Hydatidiform mole or molar pregnancy-management
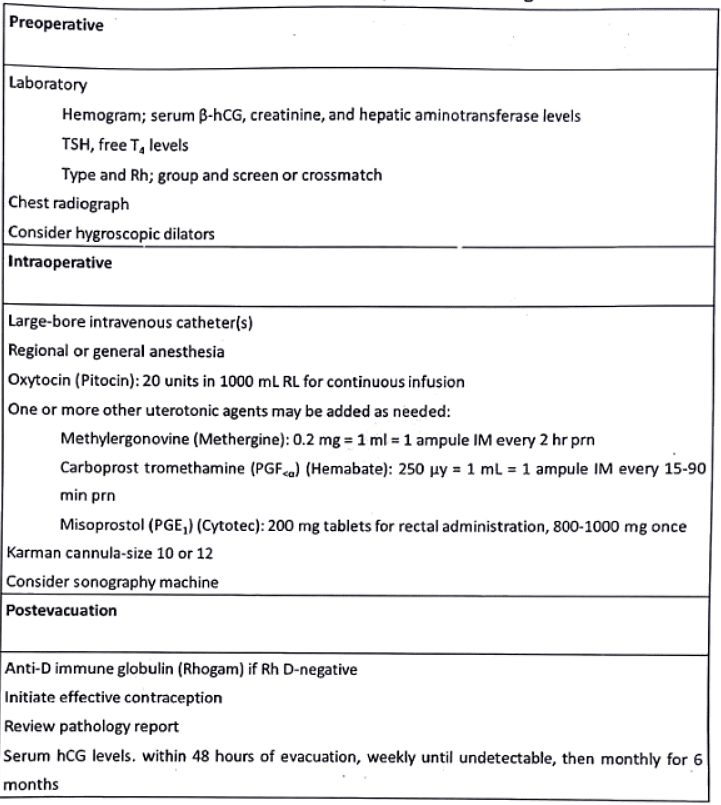
After the evacuation, the extended-term outlook for women with a hydatidiform mole does not show improvement with prophylactic chemotherapy. Consequently, the American College of Obstetricians and Gynecologists does not routinely recommend it.
Risk Factors for Trophoblastic Neoplasia Post-Molar Evacuation:
- Complete moles exhibit a 15 to 20 percent incidence of malignant consequences, whereas partial moles show a 1 to 5 percent incidence.
- Advanced age is a risk factor.
- Elevated β-hCG levels (> 100,000 mlU/mL) are associated with an increased risk.
- Larger-than-expected uterine size during gestation is a risk factor.
- The presence of theca-lutein cysts exceeding 6 cm is a risk factor.
- A slow decline in β-hCG levels is also considered a risk factor.
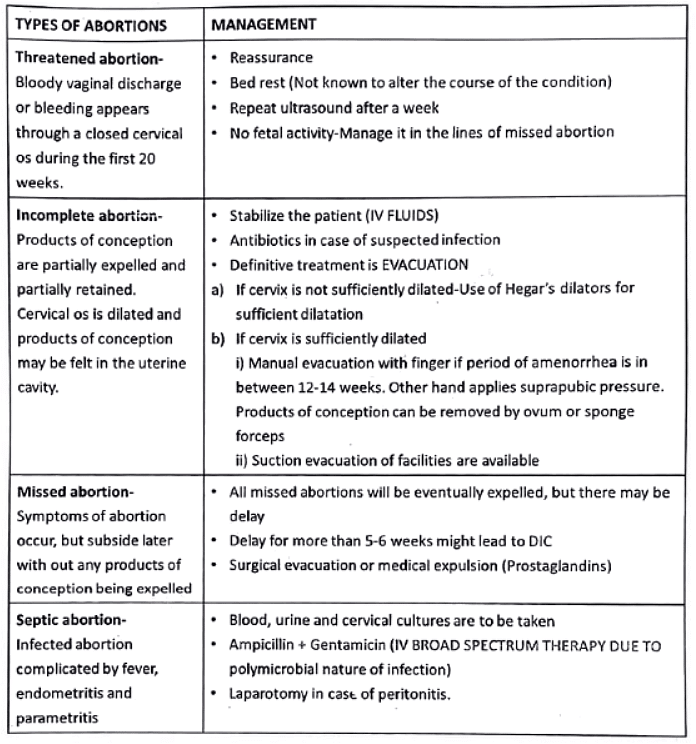
Types of abortions
MTP ACT 2020 (Amendment of MTP ACT 1971)-Bill passed in Lok sabha Mar 17, 2020
- Extension of Termination Limits: The upper limit for termination is extended to 20-24 weeks (previously 20 weeks) for cases involving rape, incest, and significant fetal anomalies.
- Determining Fetal Anomalies: A medical board comprising four members (pediatrician, radiologist, gynecologist, and a member specified by the state government) will decide on substantial fetal anomalies.
- Patient Privacy: Privacy of the patient must be maintained.
- Opinions for Termination: Up to 20 weeks, termination requires the opinion of one doctor, while 20-24 weeks necessitates opinions from two doctors.
- Partner Involvement: The term 'married woman or her husband' is replaced with 'woman or her partner' in cases of termination due to contraception failure.
- Termination Criteria by Central Government: Termination up to 24 weeks is restricted to specific categories of women as prescribed by the central government. Norms for the required medical practitioner's opinion will be notified by the central government.
- Unwanted Pregnancy Resulting from Contraception Failure: If pregnancy occurs due to contraceptive failure, it may be considered a serious threat to the mental health of the woman. The Bill replaces 'married woman or her husband' with 'woman or her partner' in this provision.
- Medical Board Constitution: The upper termination limit does not apply when necessary due to substantial fetal abnormalities diagnosed by a Medical Board. Each state government must establish a Medical Board with specified members, and the central government will outline their powers and functions.
- Protection of Privacy: Registered medical practitioners are prohibited from disclosing the identity of a woman whose pregnancy has been terminated, except to authorized individuals under the law. Violation of this provision is punishable by imprisonment or a fine.
Methods of first-trimester MTP
- Menstrual Regulation through Aspiration:
- Aspiration of the uterine cavity using Karman's cannula is effective up to 42 days from the last menstrual period (LMP).
- Potential complications include failure to evacuate, incomplete evacuation, hemorrhage, cervical laceration, perforation, infection, and anesthetic issues.
- Dilatation and Suction Evacuation (Vacuum Evacuation):
- Most effective for terminating pregnancies within the first 12 weeks.
- Utilizes a standard negative suction of 650 mm Hg for aspiration.
- Caution is advised against check curettage with a sharp curette to avoid traumatic complications like perforation, synechiae (Asherman syndrome), and the risk of placenta accreta in future pregnancies.
- Priming with prostaglandin gel or suppository helps prevent complications such as cervical tear, lacerations, and internal os injuries leading to an incompetent cervix.
- Medical Methods:
- Permissible up to 9 weeks of gestation (63 days).
- Protocol:
- Day 1: Administer 200 mg of mifepristone as a single dose. Observe the woman for half an hour and then allow her to go home. Anti-D globulin is given to RH-negative women.
- Day 3: Administer 400 mcg of oral misoprostol (prostaglandin) unless abortion has occurred. Monitor pulse and blood pressure for 2 hours. If all is well, allow the woman to go home.
- Late Sequelae of Medical Termination:
- Pelvic inflammatory disease (PID) leading to chronic pelvic pain.
- Infertility due to tubal infection and blockage.
- Incompetent cervix resulting from trauma, leading to preterm births and habitual mid-trimester abortions.
- Adherent placenta in subsequent pregnancies.
- Asherman syndrome.
- Ectopic pregnancy following PID.
- Cervical ectopic pregnancy caused by trauma.
- Intrauterine growth restriction (IUGR).
- Additional Concerns:
- Rh-isoimmunization risk if anti-D has not been administered to non-immunized Rh-negative mothers after the termination.
- Potential psychiatric disorders, especially feelings of regret or distress, may arise if the termination was performed without proper counseling, particularly if infertility follows the procedure.
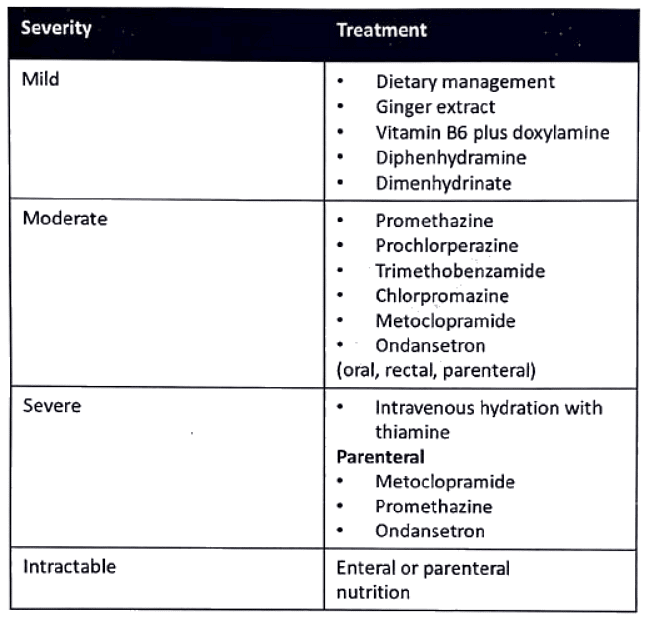
Hyperemesis gravidarum
- Hyperemesis gravidarum is intractable vomiting of pregnancy and is associated with disturbed nutrition.
- Early signs of the disorder include weight loss (up to 5% o f body weight) and ketonuria.
First trimester bleeding-Repeats
Q1: List the risk factors for ectopic pregnancy. How will you manage a 25-year old woman with ruptured tubal pregnancy (1996)?
Q2: How would you manage a case of bleeding per vaginum with pain abdomen at 8 weeks of gestation (2006)?
Q3: Discuss the differential diagnosis in a 28-year-old woman with two months amenorrhea and acute lower abdominal pain followed by bleeding per vaginum. How would you manage such patient? (2012)
Q4: A 25-year-old married lady presents with history of 10 weeks amenorrhoea, acute lower abdominal pain and fainting. On clinical examination, she has tachycardia, hypertension and pelvic tenderness (2015)
i. What is the most likely diagnosis?
ii. How would you investigate such a patient?
iii. How would you manage such a patient? List the key points.
|
7 videos|219 docs
|
FAQs on First trimester bleeding - Medical Science Optional Notes for UPSC
| 1. What are the common causes of abdominal pain during pregnancy? |  |
| 2. What is an ectopic pregnancy and how is it managed? |  |
| 3. What is a molar pregnancy and how is it managed? |  |
| 4. What are the different types of abortions? |  |
| 5. What is hyperemesis gravidarum and how is it managed? |  |