Pregnancy induced hypertension | Medical Science Optional Notes for UPSC PDF Download
Hypertensive disorders in Pregnancy
- Hypertensive disorders complicate 5-10 percent of all pregnancies
- Preeclampsia is identified in 3.9 percent of all pregnancies
Classification
- Gestational Hypertension: High blood pressure during pregnancy, but no evidence of the preeclampsia syndrome develops, and hypertension resolves by 12 weeks postpartum.
- Preeclampsia and Eclampsia Syndrome: The occurrence of the preeclampsia and eclampsia syndrome during pregnancy.
- Chronic Hypertension of Any Etiology: Persistent high blood pressure of any cause existing prior to pregnancy.
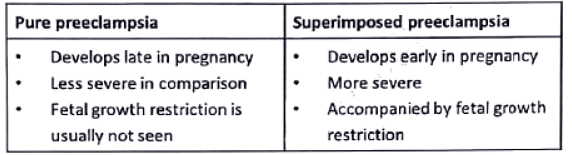
- Preeclampsia Superimposed on Chronic Hypertension: Preeclampsia syndrome developing in individuals with pre-existing chronic hypertension.
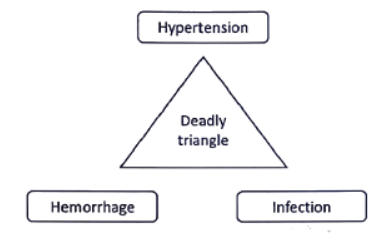
- Dangerous Nature of Preeclampsia: Preeclampsia syndrome, whether standalone or superimposed on chronic hypertension, is identified as the most perilous form.
- Gestational Hypertension Definition: Elevated blood pressure exceeding 140/90 mmHg after 20 weeks in women who were previously normotensive.
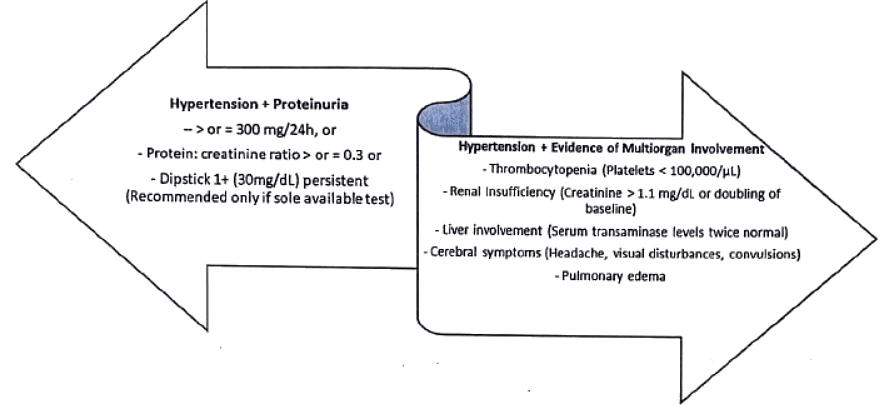
- Preeclampsia Syndrome Description:
- Describing preeclampsia as a unique pregnancy-related syndrome with the potential to impact virtually every organ system.
- Proteinuria serves as an objective marker, indicating the systemic endothelial leak characteristic of the preeclampsia syndrome.
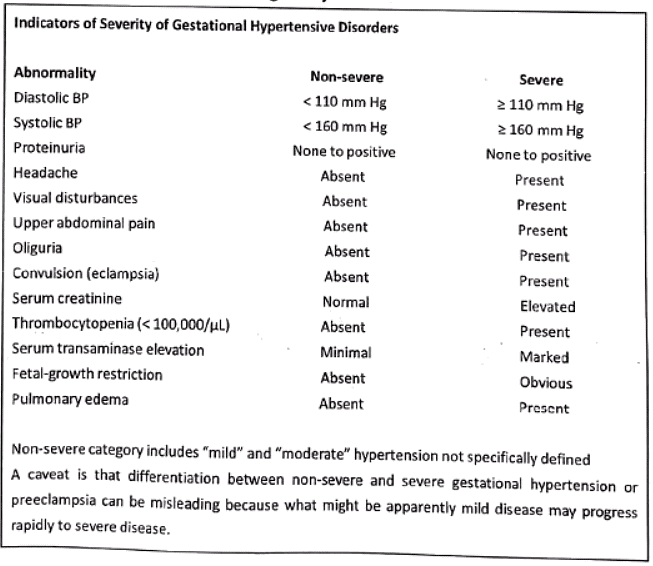
Diagnostic criteria
- Eclampsia: In the context of preeclampsia, the occurrence of an unexplained convulsion is termed eclampsia. Seizures are generalized and can manifest before, during, or after labor.
- Chronic Underlying Hypertension: The diagnosis of chronic underlying hypertension is established in women with documented blood pressures exceeding 140/90 mm Hg before pregnancy or prior to 20 weeks of gestation, or both.
- Preeclampsia Superimposed on Chronic Hypertension: If there is new-onset or worsening baseline hypertension accompanied by newly developed proteinuria or other criteria specified in the diagnostic criteria, the diagnosis of superimposed preeclampsia is made.
Delta Hypertension
A sudden rise in mean arterial pressure later in pregnancy—also known as "delta hypertension"— may also signify preeclampsia even if blood pressure is < 140/90 mm Hg. Some of these women will develop Eclamptic seizures or HELLP syndrome while still normotensive.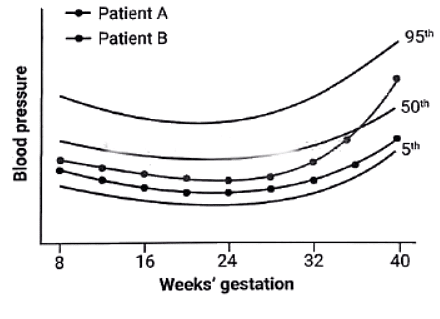
Risk Factors
- Young and nulliparous women
- Race/ethnicity/genetic predisposition
- Environmental/Seasonal/Socioeconomic factors
- Obesity
- Multifetal gestation
- Maternal age
- Hyperhomocysteinemia
- Metabolic syndrome
- History of preeclampsia in a previous pregnancy
- Surprisingly, smoking is linked to a reduced risk of hypertension during pregnancy because it upregulates placental adrenomedullin expression, which regulates volume homeostasis.
Mechanisms
- Placental implantation involving abnormal trophoblastic invasion of uterine vessels
- Immunological maladaptive tolerance between maternal, paternal (placental), and fetal tissues
- Maternal maladaptation to cardiovascular or inflammatory changes of normal pregnancy
- Genetic factors, including inherited predisposing genes and epigenetic influences
"Two-stage Disorder" Theory of Preeclampsia Etiopathogenesis
- Ness and Roberts (1996) propose the two-stage disorder comprising "maternal and placental preeclampsia."
- According to Redman and coworkers (2014), stage 1 involves faulty endovascular trophoblastic remodeling, leading to the stage 2 clinical syndrome. Stage 2 is susceptible to modification by preexisting maternal conditions such as cardiovascular or renal disease, diabetes, obesity, immunological disorders, or hereditary influences.
- This compartmentalization is artificial, and preeclampsia syndrome appears clinically as a spectrum of worsening disease.
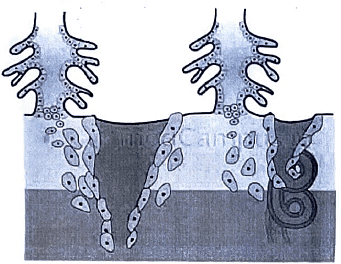
Schematic Representation of Normal Placental Implantation
- Normal implantation involves the proliferation of extravillous trophoblasts from an anchoring villus.
- These trophoblasts invade the decidua and extend into the walls of the spiral arteriole, replacing the endothelium and muscular wall to create a dilated, low-resistance vessel.
Role of Prostaglandins
- Prostacyclin Production in Preeclampsia:
- In preeclampsia, endothelial prostacyclin (PGI2) production is reduced compared to normal pregnancy.
- This reduction is mediated by phospholipase A2.
- Platelet Secretion Changes:
- Concurrently, platelets exhibit increased secretion of thromboxane A2 in preeclampsia.
- Consequently, the prostacyclin:thromboxane A2 ratio decreases.
- Effect on Sensitivity to Angiotensin II:
- The overall impact of these changes is an increased sensitivity to infused angiotensin II.
- This heightened sensitivity leads to vasoconstriction.
- These alterations become noticeable as early as 22 weeks in women predisposed to developing preeclampsia.
- HELLP Syndrome (Hemolysis, Elevated Liver Enzymes, Low Platelet Count):
- HELLP Syndrome lacks a universally accepted strict definition.
- Complications Associated with HELLP Syndrome:
- Subcapsular liver hematoma
- Eclampsia
- Placental abruption
- Acute kidney injury
- Pulmonary edema
- Stroke
- Coagulopathy
- Acute respiratory distress syndrome
- Sepsis
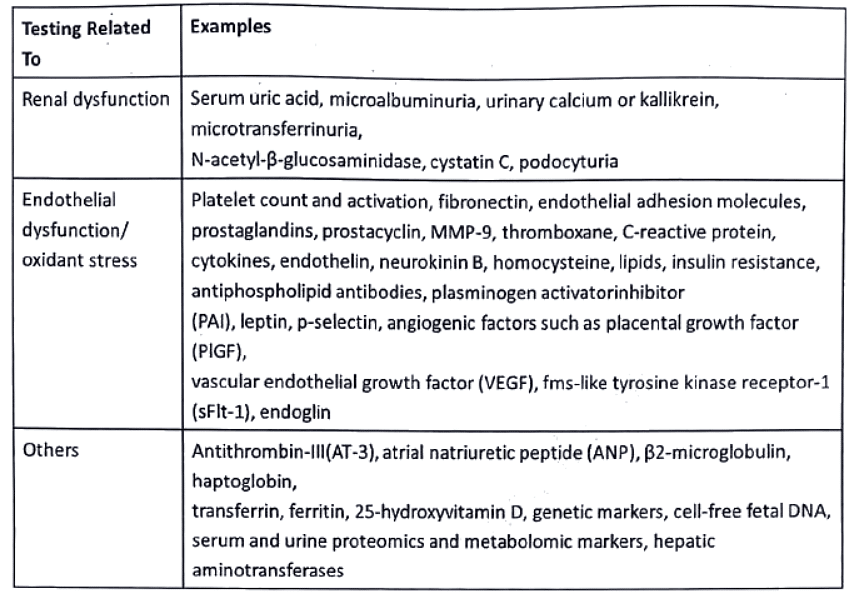
Predictive tests for the development of preeclampsia syndrome
Measurement during early pregnancy or across pregnancy of various biological, biochemical, and biophysical markers implicated in preeclampsia syndrome pathophysiology has been proposed to predict its development.
Attempts have been made to identify early markers of faulty placentation, impaired placental perfusion, endothelial cell activation and dysfunction, and activation of coagulation.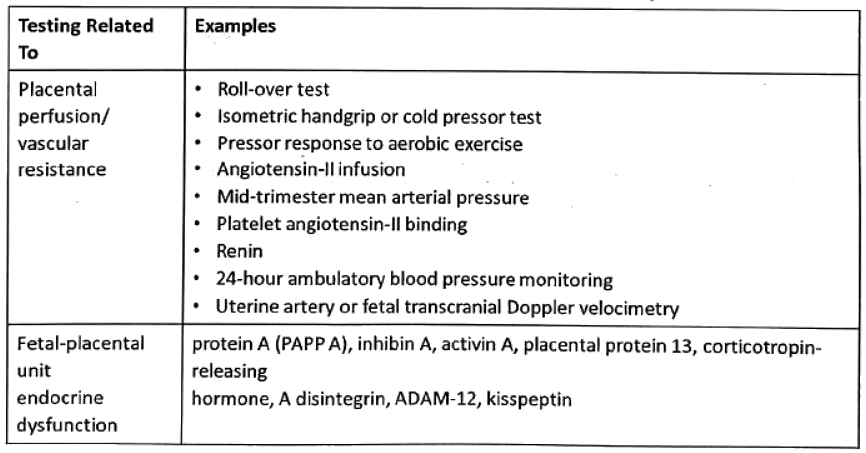
Prevention-Preeclampsia
- Dietary Manipulation: Strategies such as a low-salt diet, calcium supplementation, or fish oil supplementation have been examined in randomized trials.
- Exercise: Randomized trials have explored the impact of physical activity and stretching as preventive measures.
- Cardiovascular Drugs: Diuretics and antihypertensive drugs, classified as cardiovascular drugs, have been evaluated for their preventive potential in randomized trials.
- Antioxidants: Antioxidant supplements, including ascorbic acid (vitamin C), α-tocopherol (vitamin E), and vitamin D, have been subjects of randomized trials to assess their efficacy in preventing preeclampsia.
- Antithrombotic Drugs: Low-dose aspirin, aspirin/dipyridamole, aspirin + heparin, and aspirin + ketanserin, all categorized as antithrombotic drugs, have been investigated in randomized trials as potential preventive measures.
Management of Preeclampsia
The basic management objectives for any pregnancy complicated by preeclampsia are: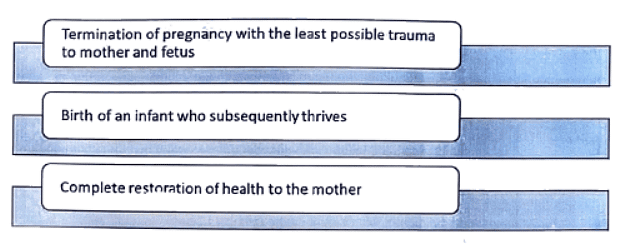
One of the most important clinical questions for successful management is precise knowledge of fetal age.
Almost certainly, the underlying disease persists until delivery is accomplished.
Termination of pregnancy is the only cure for preeclampsia
- Definitive Treatment for Preeclampsia:
- Termination of pregnancy is considered the only cure for preeclampsia.
- Early Diagnosis Measures:
- Early diagnosis of preeclampsia is facilitated by an increased frequency of prenatal visits.
- Outpatient Management for Mild Disease:
- Women with mild preeclampsia can often be managed as outpatients.
- Hospitalization Criteria:
- Hospitalization is recommended upon the development of proteinuria.
- Systematic Evaluation After Admission:
- Detailed examination, daily weight determination, and urine analysis (proteinuria/urine protein-creatinine ratio) on admission day and subsequent days.
- Regular Monitoring:
- Regular monitoring includes blood pressure checks and assessments of liver function (LFT), renal function (RFT), and complete blood count (CBP).
- Evaluation of Fetal Well-being:
- Assessment of fetal size and well-being, along with amniotic fluid index (AFI) measurement.
- Reduced Physical Activity:
- Mild cases are generally managed conservatively until labor begins spontaneously.
- Severe cases may require anticonvulsant and antihypertensive therapy followed by delivery, depending on disease severity and fetal age.
- Induction of Labor:
- Induction of labor and vaginal delivery are traditionally considered ideal for severe preeclampsia.
- Cesarean delivery is indicated when induction is unlikely to succeed or has failed.
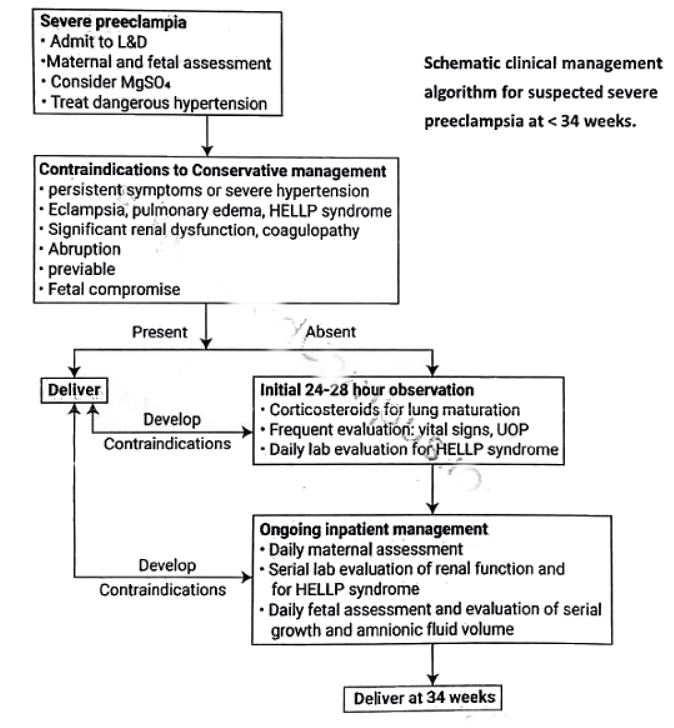
Delayed delivery- "conservative" or "expectant" management
- Historical Practice:
- Until the early 1990s, the standard practice was immediate delivery for all women diagnosed with severe preeclampsia.
- Evolution of Approach:
- Over the past 25 years, an alternative approach has been proposed for women with preterm severe preeclampsia.
- Conservative or Expectant Management:
- This newer approach involves "conservative" or "expectant" management, aiming to enhance neonatal outcomes without compromising maternal safety.
- Termination Guidelines Based on Gestational Age:
- For severe preeclampsia before 23 weeks, termination of pregnancy is recommended.
- Between 24-34 weeks, studies do not overwhelmingly favor one approach over the other—expectant management versus immediate delivery.
- Primary Consideration:
- The primary consideration for terminating pregnancies with severe preeclampsia is maternal safety.
- No data suggest that expectant management provides benefits for the mother.
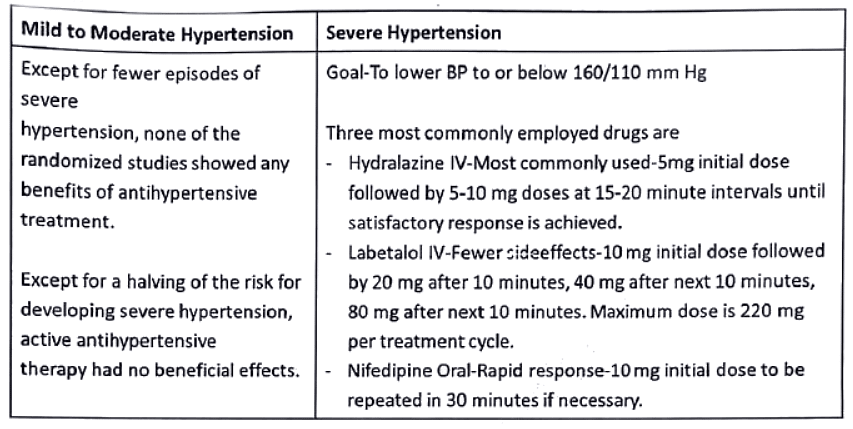
Antihypertensive therapy
Differential Diagnosis
Conditions to consider in the differential diagnosis of seizures include epilepsy, encephalitis, meningitis, brain tumor, neurocysticercosis, amniotic fluid embolism, postdural puncture cephalgia, and ruptured cerebral aneurysm.
 |
Download the notes
Pregnancy induced hypertension
|
Download as PDF |
Immediate Seizure Management
Immediate measures for managing a seizure involve protecting the airway and preventing tongue bites.
Prophylaxis and Treatment of Seizures
- Magnesium sulfate is the treatment of choice for both prophylaxis and management of seizures.
- During labor and delivery, women with preeclampsia-eclampsia are commonly administered magnesium sulfate. This is continued for 24 hours postpartum.
- It's important to note that magnesium sulfate is not used to treat hypertension.
- An advantage of magnesium sulfate is its avoidance of central nervous system depression in both the mother and the infant.
Magnesium Sulfate Neuroprophylaxis
- The 2013 Task Force recommends the use of magnesium sulfate neuroprophylaxis for women with eclampsia or severe preeclampsia.
Parkland Hospital Criteria for New-Onset Proteinuric Hypertension
- In a woman with new-onset proteinuric hypertension, at least one of the following criteria is required:
- Systolic BP > 160 or diastolic BP > 110 mm Hg
- Proteinuria > 2+ by dipstick in a catheterized urine specimen
- Serum creatinine > 1.2 mg/dL
- Platelet count < 100,000/pL
- Elevated aspartate aminotransferase (AST) two times above the upper limit of the normal range
- Persistent headache or scotomata
- Persistent mid-epigastric or right-upper quadrant pain
Continuous IV infusion of Magnesium sulfate
- Magnesium Sulfate Administration:
- Magnesium sulfate can be given either intravenously through continuous infusion or intramuscularly with intermittent injection.
- Preference for Intravenous Route:
- Intravenous administration is the preferred and widely adopted method, with intramuscular use being largely abandoned in most units.
- Effectiveness of Intramuscular Administration:
- It's important to note that intramuscular administration is equally effective as intravenous administration.
- Continuous IV Infusion Procedure: For continuous intravenous infusion of magnesium sulfate:
- Administer a loading dose of 4 to 6 grams diluted in 100 mL of intravenous fluid over 15-20 minutes.
- Initiate a maintenance infusion of 2 grams per hour in 100 mL of intravenous fluid.
- Monitor for magnesium toxicity, including periodic assessment of deep tendon reflexes.
- Some practitioners measure serum magnesium levels at 4-6 hours and adjust the infusion to maintain levels between 4 and 7 mEq/L (4.8 to 8.4 mg/dL).
- Discontinue magnesium sulfate 24 hours after delivery.
Pritchards regimen-intermittent Intramuscular injections
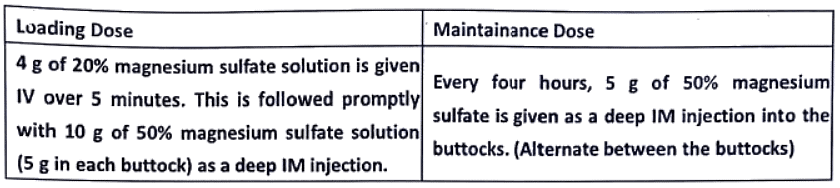
The treatment is continued for 24 hours after delivery or the last convulsion, whichever occurs later.
Monitoring of the therapy for signs of toxicity
- Monitoring for Signs of Toxicity:
- Regular monitoring for signs of toxicity during magnesium sulfate therapy is crucial.
- Respiratory Rate:
- Maintain a respiratory rate of at least 16 per minute.
- In cases of mild to moderate respiratory depression, treatment involves intravenous administration of 1 g calcium gluconate or calcium chloride. Further magnesium sulfate is usually withheld.
- Patellar Reflexes:
- Patellar reflexes should be present during therapy.
- Loss of patellar reflexes, typically occurring at serum magnesium levels of 10-12 mEq/L, is an early indication of magnesium sulfate toxicity.
- Urinary Output:
- Ensure a urinary output of at least 30 ml per hour over the last four hours.
- Withholding Criteria:
- If any of these monitoring criteria are not fulfilled, the administration of the drug is withheld.
- Respiratory Arrest Management:
- In cases of respiratory arrest, calcium gluconate is used as an antagonist to reverse the effects of magnesium sulfate.
Management of Eclampsia-Principles of Management
In antepartum eclampsia, labor may begin spontaneously shortly after convulsions ensue and may progress rapidly.
If the convulsions occur during labor, contractions may increase in frequency and intensity, and the duration of labor may be shortened.
Principles of Management
- Control of convulsions using an intravenously administered loading dose of magnesium sulfate that is followed by a maintenance dose, usually intravenous, of magnesium sulfate.
- Intermittent administration of an antihypertensive medication to lower blood pressure whenever it is considered dangerously high.
- Avoidance of diuretics unless there is obvious pulmonary edema, limitation of intravenous fluid administration unless fluid loss is excessive, and avoidance of hyperosmotic agents.
- Delivery of the fetus to achieve a remission of preeclampsia.
Pregnancy induced Hypertension-Repeats
Q1: Define high risk pregnancy. Discuss the management of a primi gravida at 36 weeks of gestation with BP of 150/100 mm Hg and one plus albuminuria (1994).
Q2: Describe the diagnosis and management of pregnancy induced hypertension at 38 weeks of gestation (2000)
Q3: Discuss the management of Eclampsia in Primi gravida at 37 weeks of gestations (2002).
Q4: How will you manage a case of severe preeclampsia in a primi gravida at 34 weeks of pregnancy (2004)?
Q5: Describe the management of pregnancy induced severe hypertension. (2010)
Q6: What is Gestational Hypertension? What is superimposed pre-eclampsia? What is the role of antihypertensive in pre-eclampsia? (2019)
|
7 videos|219 docs
|